Newsletter 2023
Newsletter July 2023: Follow up on the 2020 ESAIC Research Project Grant winning project and 2020 ESAIC Support Grant winner
In this review, we explore the progress and outcomes of two significant projects supported by the ESAIC in 2020. The first project, the ESAIC Research Project Grant, was awarded to Wolfgang Buhre from the Netherlands, with the aim of facilitating groundbreaking research in the field of anaesthesiology and intensive care. The second project, the ESAIC Support Grant, was awarded to Martin Scharffenberg from Germany, with the purpose of providing assistance for research in the same field. The results of these projects have generated great anticipation among researchers and practitioners alike. These projects highlight the potential of innovative research in enhancing patient care and improving outcomes within the fields of anaesthesiology and intensive care. The findings derived from these studies hold the promise of far-reaching implications for clinical practice and patient management in the years to come.
ESAIC Research Project Grant 2020
Prevention of persistent pain after breast cancer treatment by online cognitive behavioural therapy
Anne Lukas, Maurice Theunissen, Dianne de Korte-de Boer, Sander van Kuijk, Walter Magerl, Werner Mess, Madelon Peters & Wolfgang Buhre
Background: Surviving breast cancer does not necessarily mean complete recovery to a premorbid state of health. Amongst the multiple psychological and somatic symptoms that reduce the quality of life of breast cancer survivors, persistent pain after breast cancer treatment (PPBCT) with a prevalence of 15-65% is probably the most invalidating [1] [2]. Several Patient- and treatment-related risk factors for PPBCT have been identified in the past decades. Patient-related risk factors such as genetic haplotypes, younger age, high BMI, pre-existing pain, high postoperative pain intensity and psychological distress suggest a greater vulnerability of a nociceptive system that is prone to sensitization [3] [4] [5]. Many interventions aiming at reducing PPBCT prevalence by decreasing nociceptive input and concomitant sensitization of the central nociceptive system have been investigated with negligible effect despite good acute postoperative pain relief [6] [7]. Only three pilot studies have been performed to modify psychological distress around breast cancer surgery [8] with minimal yet detectable effects on postoperative pain intensity, opioid consumption and psychological distress.
The AMAZONE study aims to investigate the effect of five perioperative sessions of online cognitive behavioural therapy (e-CBT), offered to patients scoring high for psychological distress, on the prevalence of PPBCT six months after surgery.
Methods: The AMAZONE study is a multicenter randomized controlled trial with an additional control arm. Patients (n=138) scheduled for unilateral breast cancer surgery scoring high for psychological distress (PD) are randomized to receive either five sessions of e-CBT or an online sham intervention consisting of information about the surgery and a healthy lifestyle (EDU) (figure 1). In addition to the online sessions, patients have three manualized online appointments with a psychotherapist to monitor and sustain the intervention and increase motivation. Patients with low PD (n~322) receive treatment as usual (TAU, additional control arm).
The primary endpoint is PPBCT incidence six months after surgery. Secondary endpoints are PPBCT intensity and interference at two, six and 12 months, the intensity of acute postoperative pain during the first week after surgery, cessation of postoperative opioid use, the sensitivity of the nociceptive and non-nociceptive somatosensory system (QST), the efficiency of endogenous pain modulation (CPM), quality of life and psychological distress.
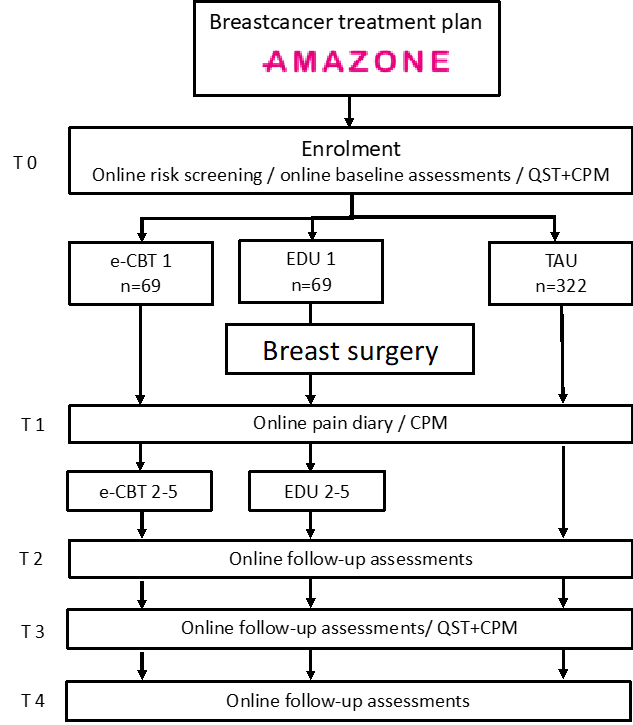
Figure 1: Time schedule of enrolment
T0: 1-3 weeks pre-surgery, T1: postoperative week, T2: 2 months follow-up, T3: 6 months follow-up, T4: 12 months follow-up. e-CBT online cognitive behavioural therapy EDU online educational therapy, TAU treatment as usual. QST quantitative sensory testing, CPM conditioned pain modulation
State of the study in Spring 2023
Like with most clinical studies, recruitment and conduction of the AMAZONE study were affected by the SARS-CoV-2 pandemic. The first patient was included in June 2021, and until now, 252 patients have been enrolled. Of these, 38 were randomized to e-CBT, 41 to EDU and 146 were TAU. Thirty-four patients had to be excluded – mostly because of surgery scheduling problems during the pandemic. Sensitivity and CPM testing could not be performed until April 2022. To compensate for the pandemic restrictions and burden on the involved staff, a lot of effort was put into interacting with and supporting the six study centres to keep the team spirit up and inclusion going.
The first interim analyses revealed a good to very good quality and feasibility of e-CBT. The contact with the therapists was experienced as sufficient and supportive, and all patients said they would recommend the intervention to others. Two months after surgery, the incidence of persistent postoperative pain was higher in patients with PD. However, e-CBT reduces it almost to the level of patients without PD compared to EDU (figure 2).
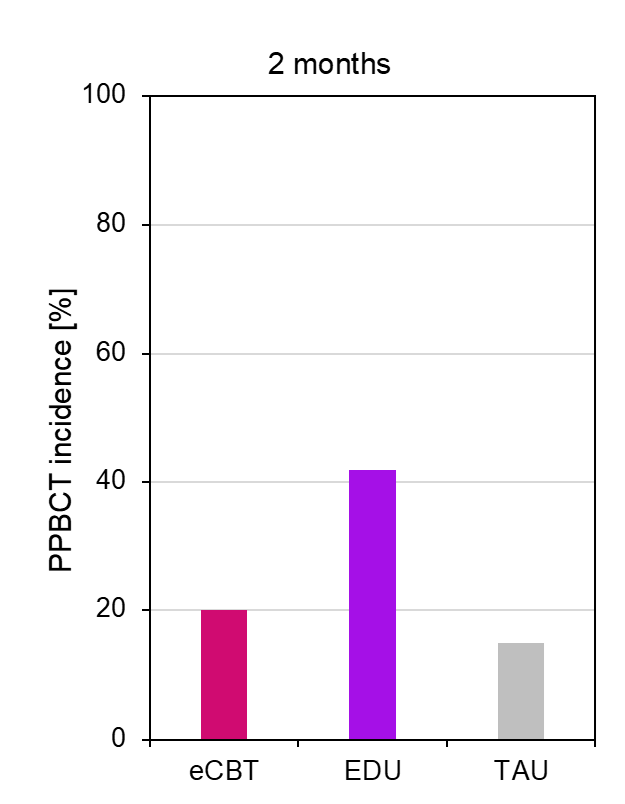
Figure 2: Incidence of PPBCT two months after surgery
e-CBT n=25, EDU n=24 and TAU n=90 patients
Conclusion
AMAZONE is one of the first studies addressing psychological distress to prevent persistent pain after breast cancer treatment. The intervention is offered online only to patients scoring high for psychological distress before surgery, thus embracing the concept of individualized patient-tailored medicine. The internet-based AMAZONE e-CBT intervention proved particularly useful during the SARS-CoV-2 pandemic, in addition to the intended advantage of sparing patients from extra appointments in an already burdensome period. The first results are promising as the AMAZONE e-CBT intervention seems feasible and effective.
References
- Tait R.C., et al. J Pain 2018; 19(12): 1367-1383.
- Bell R.J., et al. J Cancer Surviv 2014; 8(1): p. 1-8.
- Theunissen M., et al. Clin J Pain 2012; 28(9): p. 819-41.
- Bruce J. et al. Pain 2014; 155(2): p. 232-43.
- Leysen L, et al. Pain Pract 2019; 19(2): p. 183-195.
- Maniker RB, et al. Curr Pain Headache Rep 2022; 26(4): p. 299-321.
- Chen Y.K., et al. Anaesthesia 2021; 76 Suppl 1(Suppl 1): p. 8-17.
- Nadinda P.G., et al. Pain 2022; 163(7): p. 1254-1273.
ESAIC Support Grant 2020
Mechanical power and pulmonary neutrophilic inflammation during lung protective ventilation strategies – A proof-of-concept pilot experimental study on the mechanisms of ventilator-induced lung injury
Martin Scharffenberg, Jakob Wittenstein, Xi Ran, Yingying Zhang, Anja Braune, Raphael Theilen, Lorenzo Maiello, Giulia Benzi, Paolo Pelosi, Patricia R. M. Rocco, Marcus J. Schultz, Jörg Kotzerke, Robert Huhle, Marcelo Gama de Abreu
Background
Known as ventilator-induced lung injury (VILI), mechanical ventilation (MV) may cause lung injury 1. VILI may be linked to the energy that is inevitably transferred to the respiratory system during MV, which can be expressed as mechanical power (MP) when multiplied by respiratory rate (RR) 2. First mentioned in 2010 3, the concept gained attention in recent years 2,4,5. We aimed to investigate MP during clinically relevant lung-protective MV strategies and its relation to pulmonary neutrophilic inflammation as assessed by positron-emission tomography (PET/CT) in a model of acute lung injury in pigs.
Experimental Protocol
Twenty-four juvenile pigs were anaesthetized and instrumented. Lung injury was induced by surfactant depletion and followed by an initial PET scan. Animals were randomized to receive low tidal volume ventilation (6 ml/kg) according to either 1) the Open Lung Approach with repeated lung recruitment manoeuvres and compliance-optimized PEEP (OLA), 2) the ARDS network high positive end-expiratory pressure (PEEP) table (HighPEEP), or 3) the ARDS network low PEEP table (LowPEEP) (n=8/group). RR was titrated to keep pH>7.15. Physiological measurements were conducted every six h. Lung imaging was repeated 24 h after the initial PET/CT. We assessed pulmonary neutrophilic inflammation by normalized uptake rate of 2-deoxy-2-[18F]fluoro-D-glucose (KiS) and calculated its difference between the two PET/CT (∆KiS). MP was derived by calculating mechanical energy via numerical integration of recorded pressure-volume curves and multiplication with RR. Statistics included non-parametric tests, a general linear model and Spearman correlation (α=0.05).
Main Results
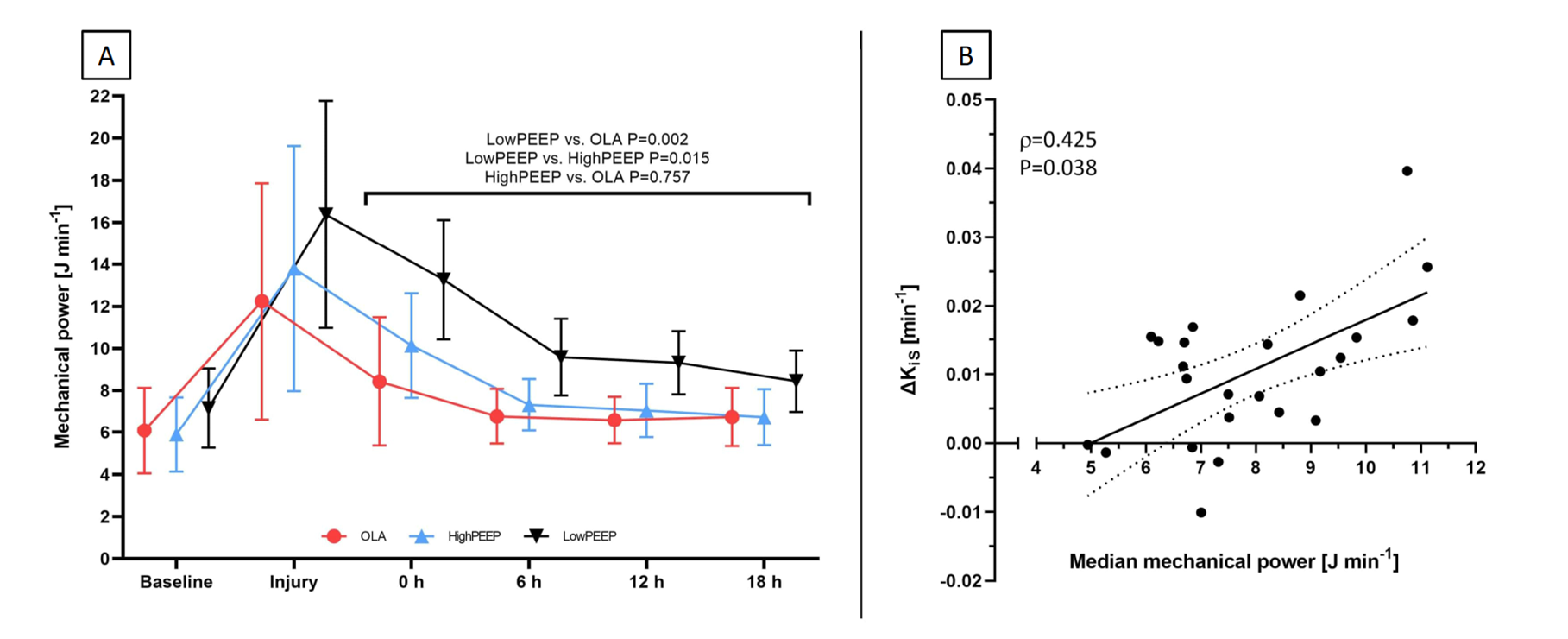
Surfactant depletion significantly impaired PaO2/FIO2 (mean±SD, 113±33 mmHg). During intervention time, median PEEP was significantly lower in LowPEEP (5;0.1 cmH2O) than in HighPEEP (12;0.2 cmH2O; P<0.001) and OLA (12;2.0 cmH2O; P<0.001). Driving pressure (P<0.001) and elastance (P=0.001) were higher in LowPEEP than in the other groups. MP was significantly higher during LowPEEP than HighPEEP and OLA (Fig.1A). ∆KiS was higher in LowPEEP (0.0183±0.0109 min-1) than in OLA (0.0049±0.0088 min-1; P=0.024), but did not differ between LowPEEP and HighPEEP (0.0080±0.0073 min-1; P=0.104) or HighPEEP and OLA (P=0.876). MP correlated significantly with ∆KiS (Fig.1B). RR (P=0.007) and PaO2/FIO2 (P=0.001) was significantly lower in LowPEEP than in OLA but did not differ between HighPEEP and OLA. Cardiac output and mean arterial pressure did not differ, while the total dose of norepinephrine was significantly higher in OLA than in LowPEEP (P=0.033).
Limitations and Potential Clinical Implications
The surfactant depletion-based injury model, and the selected VILI surrogate may limit the generalizability of the obtained results. However, we gained valuable data on MP transferred during clinically relevant lung-protective MV concepts and the link between MP and VILI. Because MP was associated with a major pathological mechanism in acute respiratory distress syndrome, namely neutrophilic infiltration and inflammation, clinicians may consider adjusting MV to minimize MP while providing acceptable gas exchange. In this regard, OLA did not outperform MV according to the ARDS network’s high PEEP table but caused higher vasopressor utilization.
Conclusion
In this experimental acute lung injury model in pigs, MP was highest during low PEEP ventilation and associated with increased pulmonary neutrophilic inflammation.
References
- Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126-2136. doi:10.1056/NEJMra1208707
- Cressoni M, Gotti M, Chiurazzi C, et al. Mechanical Power and Development of Ventilator-induced Lung Injury. Anesthesiology. 2016;124(5):1100-1108. doi:10.1097/ALN.0000000000001056
- Guttmann J. Energietransfer Beatmungsgerät-Patient – Kann man das weiter minimieren? Anästh Intensivmed. 2010;(51):527.
- Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567-1575. doi:10.1007/s00134-016-4505-2
- Serpa Neto A, Deliberato RO, Johnson AEW, et al. The mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914-1922. doi:10.1007/s00134-018-5375-6
Funding: This study was funded by the ESAIC Research Support Grant 2020, a grant from the German Research Foundation (DFG; GA 1256/8-1DFG), and a grant by the local Faculty of Medicine Carl Gustav Carus, Dresden, Germany (MeDDrive #60439).
Figure 1, A: Mechanical power during the experimental time course (left panel), and B: Correlation between median mechanical power and ∆KiS (right panel). OLA, Ventilation according to open lung approach; HighPEEP, Ventilation using the ARDS network high PEEP table; LowPEEP, Ventilation using the ARDS network low PEEP table; ∆KiS, Change in tissue-normalized 2-deoxy-2-[18F]fluoro-D-glucose uptake rate
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter”]