Newsletter 2023
Newsletter July 2023: Follow up on the two ESAIC Grant winners from 2020 Young Investigator grants
In this detailed review, we explore the progress and outcomes of two noteworthy research projects that received the Young Investigator Start-up Grants from the ESAIC in 2020. Francesca Dalla Corte from Italy and Christina Massoth from Germany were the recipients of these grants, which aimed to promote innovative research in the fields of anaesthesiology and intensive care. The research projects funded by these grants have generated significant interest within the medical community.
ESAIC Young Investigator Start-up Grant 2020
Adherence to AKI guidelines in clinical practice – still a long way to go?
More than a decade ago, the Kidney Disease Improving Global Outcomes (KDIGO) guidelines proposed a care bundle comprising six measures for patients at risk for or with acute kidney injury (AKI). 1 Ever since, a growing body of evidence consisting of quality improvement initiatives and randomized controlled trials emerged, supporting the efficacy of this care bundle to reduce the incidence of moderate and severe AKI. 2–5
Since a causal treatment for AKI remains to be found, implementing the KDIGO recommendations represents the therapeutic mainstay to mitigate the morbidity and mortality associated with AKI. Patients undergoing cardiac surgery have a particularly high risk of developing postoperative AKI, with an incidence of 20% to 40%. 6,7 To assess guideline compliance in clinical practice in this at-risk population, we conducted this observational study at six international institutions. Our primary endpoint was the proportion of cardiac surgery patients receiving the complete care bundle consisting of the following measures: discontinuation of nephrotoxic medication when possible, tight glycemic control, close monitoring of serum creatinine and urine output, optimization of hemodynamic parameters and volume status, implementation of functional hemodynamic monitoring and avoidance of radiocontrast agents.
In total, 537 patients undergoing cardiac procedures were enrolled in the study, of whom 27.2% developed AKI within 72 hours after surgery. The complete care bundle of all six measures was implemented in 0.4% of patients. Nephrotoxic drugs were discontinued in 15.6% of patients, hyperglycemia was avoided in 39.6%, and another 6.3% received intensified monitoring of renal function. Volume status and hemodynamics were optimized in 57.4%, afunctional hemodynamic monitoring was applied in 43.9%, and radiocontrast agents were successfully avoided in 95.3%. Patients received, on average, 2.6 (SD 1.0) measures of the bundle irrespective of whether they developed AKI or not (p=0.854). 8
Our findings exposed a very low adherence to the measures recommended by the KDIGO guidelines in patients undergoing cardiac surgery. Poor compliance is a well-known problem in clinical care and has been described extensively for some conditions, such as treating sepsis. 9,10 Similarly, our survey implies a need for educational programs and quality improvement initiatives to enhance the implementation of the KDIGO guidelines in clinical routine, thereby decreasing the financial costs and morbidity associated with AKI.
References
- Kellum JA, Lameire N, Aspelin P et al. KDIGO Clinical Practice Guideline for Acute Kidney Injury 2012. Kidney International Supplements 2012; 2:1–138.
- Göcze I, Jauch D, Götz M, et al. Biomarker-guided Intervention to Prevent Acute Kidney Injury After Major Surgery: The Prospective Randomized BigpAK Study. Annals of surgery 2018; 267:1013–1020.
- Meersch M, Schmidt C, Hoffmeier A, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high-risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Medicine 2017; 43:1551–1561.
- Zarbock A, Küllmar M, Ostermann M, et al. Prevention of Cardiac Surgery-Associated Acute Kidney Injury by Implementing the KDIGO Guidelines in High-Risk Patients Identified by Biomarkers: The PrevAKI-Multicenter Randomized Controlled Trial. Anaesthesia and analgesia 2021; 133:292–302.
- Engelman DT, Crisafi C, Germain M, et al. Using urinary biomarkers to reduce acute kidney injury following cardiac surgery. Journal of Thoracic and Cardiovascular Surgery 2020; 160:1235-1246.e2.
- Hu J, Chen R, Liu S, et al. Global Incidence and Outcomes of Adult Patients With Acute Kidney Injury After Cardiac Surgery: A Systematic Review and Meta-Analysis. Journal of Cardiothoracic and vascular anaesthesia 2016; 30:82–9.
- Lagny M-G, Jouret F, Koch J-N, et al. Incidence and outcomes of acute kidney injury after cardiac surgery using either criteria of the RIFLE classification. BMC nephrology 2015; 16:76.
- Massoth C, Küllmar M, Moncho AP, et al. Implementation of the Kidney Disease Improving Global Outcomes guidelines for the prevention of acute kidney injury after cardiac surgery: An international cohort survey. European Journal of Anaesthesiology 2023.
- Leone M, Ragonnet B, Alonso S, et al. Variable compliance with clinical practice guidelines was identified in a 1-day audit at 66 French adult intensive care units. Critical care medicine 2012; 40:3189–95.
- Bitton E, Zimmerman S, Azevedo LCP, et al. An international survey of adherence to Surviving Sepsis Campaign Guidelines 2016 regarding fluid resuscitation and vasopressors in the initial management of septic shock. Journal of critical care 2022; 68:144–154.
ESAIC Young Investigator Start-up Grant 2020
An ongoing randomized controlled trial on High Flow Nasal Cannula use after thoracic surgery: any effect on diaphragmatic function and postoperative pulmonary complications?
Dalla Corte F, Fogagnolo A, Ragazzi R, Benetto G, De Paoli G, Piccioni F, Volta CA, Spadaro S
Background and Goal of Study: Postoperative diaphragmatic dysfunction (DDys) is frequent after thoracic surgery (TS) and is associated with a higher incidence of postoperative pulmonary complications (PPCs) [1]. PPCs incidence after thoracic surgery ranges from 19 to 59%. It leads to increased healthcare costs, primarily due to increased length of stay (LOS) and intensive care unit (ICU) admission.
The ultrasound (US) technique has recently emerged as a point-of-care tool to detect DDys [2]. High Flow Nasal Cannula (HFNC) is a non-invasive respiratory support that can improve oxygenation and reduce the work of breathing [3]. However, in recent literature, there are no clear indications of HFNC use in the perioperative setting [4]. We hypothesized that HFNC could reduce the prevalence of DDys after we assessed TS and reduce the incidence of PPCs compared to standard oxygenation therapy (SOT).
Materials and Methods: Patients ≥ 18 years old scheduled for major lung resection surgery in video-assisted TS were enrolled. Two hours after extubation (T0), patients were randomized to receive either HFNC or SOT for 24 hours. The diaphragmatic function was assessed by ultrasound on the first (T1) and second (T2) postoperative day. Both diaphragmatic displacement (DD) and thickening fraction (TF) were assessed bilaterally with DD < 1 cm and TF < 30%, indicating DDys [5]. A strong diaphragmatic effort was defined as a TF > 40% [6]. The incidence of PPCs was recorded daily from the 1st to the 7th postoperative day. Postoperative analgesia was ensured with acetaminophen, NSAIDs boluses, and morphine as adjunctive therapy if the pain Visual Analogic Score (VAS) was > 4. Patients’ comfort (1 poor to 5 excellent) and Borg dyspnoea scale were also assessed.
Results and Discussion: A total of 93 patients were included, 44 in the HFNC and 49 in the SOT groups. The total sample size is expected to be 116 patients (58 per group); so far, seven patients have been lost to follow-up. Patients had mostly an ASA score of 3 (75/94, 80%), and the median ARISCAT score was 49 [42-49]. The clinical characteristics of the two groups were similar.
A bilateral DD < 1 cm was found in 20% and 13% of patients at T1 and T2, respectively. A bilateral TF < 30% was found in 14% and 9% of patients at T1 and T2, respectively. No statistically significant differences were found between the two groups.
On the operated side, the prevalence of TF < 30% was comparable between the two groups both at T1 (35% vs 39%, p=.708) and at T2 (24% vs 17%, p=.414). A strong diaphragmatic effort of the not operated side was less frequent in the HFNC vs SOT group both at T1 (43% vs 55%, p=.244) and T2 (54% vs 61%, p=.454).
VAS pain scale ranged between 1 and 7 at T1 and 1 and 3 at T2, with no statistically significant differences between the two groups. Comfort was comparable between the two groups ranging between 2 and 5 overall. The Borg dyspnoea score was comparable as well.
PPCs incidence was 44% (19/43) in the HFNC group vs 63% (31/49) in the SOT group (p = .067).
Conclusion(s): HFNC therapy is a useful and tolerable device after TS. The effect on diaphragmatic function is still unclear, and its ability to reduce Ddys is still under debate. Diaphragmatic ultrasound and its cut-off for diaphragmatic dysfunction should be used cautiously in the perioperative setting. Therefore, additional studies should be performed to assess whether HFNC might reduce Ddys prevalence and PPCs incidence.
References
- Miskovic A, Lumb AB. Br J Anaesth 2017;118:317-334;
- Spadaro S, Grasso S, Dres M et al. Anesthesiology 2019;131:266–278;
- Mauri T, Wang YM, Dalla Corte F et al. Open Access Emerg Med 2019;11:109-120.
- Oczkowski S, Ergan B, Bos L, et al. Eur Respir J 2022;59:2101574.
- Zambon M, Greco M, Bocchino S et al. Intensive Care Med 2017;43:29–38.
- Umbrello M, Formenti P, Longhi D, et al. Crit Care 2015;19:161.
Funding: The present study was funded by the EASIC Young Investigator Start-up Grant 2020.
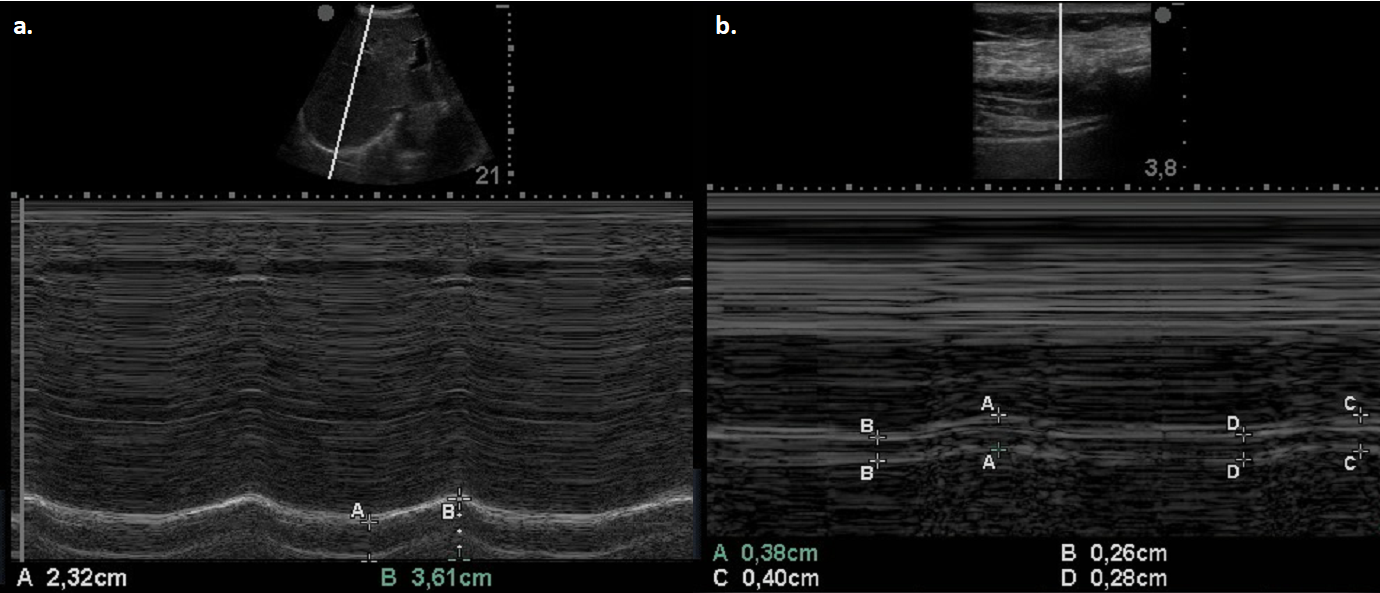
Figure 1. Two representative pictures in M-mode ultrasound of diaphragmatic displacement (a.) and thickening fraction (b.)
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter”]










