Newsletter 2023
ESAIC focused guideline for the use of cardiac biomarkers in perioperative risk evaluation
Giovanna Lurati Buse, Bernardo Bollen Pinto, Michelle S Chew
The “ESAIC focused guideline for the use of cardiac biomarkers in perioperative risk evaluation” has recently been published in the European Journal of Anaesthesiology 34(4):p 192-214, April 2017, following feedback from all ESAIC members and approval from relevant ESAIC bodies.
Numerous publications on cardiac biomarkers, specifically cardiac troponin and B-type natriuretic peptides, have raised awareness of the impact of myocardial injury. The lack of clarity on how to interpret and utilise these biomarkers in perioperative care has made it necessary to develop this focused guideline.
The guideline aims to provide updated guidance on measuring cardiac biomarkers in adults undergoing non-cardiac surgery, covering the following areas of application:
| SCOPE OF APPLICATION | CLINICAL QUESTION |
| Prognosis | How do elevated biomarker concentrations influence the risk of specific outcomes? |
| Prediction | How much does the biomarker contribute to the differentiation of patients with and without specific events? |
| Biomarker-enhanced management | Do systematic biomarker measurements and derived perioperative interventions improve outcomes? |
The guidelines addressed measurements of cardiac troponin and B-type natriuretic peptides, both before and after surgery or in combination (dynamics).
The task force conducted a comprehensive literature search, yielding over 25,000 results. The recommendations were based on a body of evidence derived from 115 full-text articles. The task force carefully analysed these articles to identify data on the association between cardiac troponin or B-type natriuretic peptides and 12 outcomes deemed critical for perioperative care (prognosis). Additionally, they evaluated prediction measures (such as discrimination and calibration measures) for the same outcomes and considered potential studies that reported interventions triggered by biomarker measurements.
Critical outcomes identified by the task force on cardiac biomarkers using a modified Delphi method
| All-cause mortality up to 30 days after surgery |
| All-cause mortality up to 1 year after surgery |
| Cardiac mortality up to 30 days after surgery |
| Death or myocardial infarction up to 30 days after surgery |
| Death or myocardial infarction up to 1 year after surgery |
| Major adverse cardiac events up to 30 days after surgery |
| Major adverse cardiac events up to 1 year after surgery |
| Cardiac complications of any severity up to 30 days after surgery |
| Myocardial injury up to 30 days after surgery (detected by systematic troponin screening; not fulfilling 4th universal definition of myocardial infarction) |
| Complications (cardiac and noncardiac) up to 30 days after surgery |
| Short-term disability using a predefined scale/scoring system (collected up to 90 days after surgery) |
| Short-term Quality of Life (collected up to 90 days after surgery). |
In accordance with the framework of the ESAIC guidelines committee, the task force prepared the guidelines following the GRADE methodology. This means that, apart from evaluating the overall certainty of evidence across all critical outcomes (defined using a Delphi process), the panellists specifically considered and assessed the following factors when formulating the recommendations:
- The balance between desirable and undesirable effects.
- The balance between health gains and resource requirements.
- Impact on health inequities.
- Acceptability to key stakeholders.
- Feasibility of implementation.
The evaluation of the available evidence revealed the following:
- There was variability in the certainty of evidence across different critical outcomes. For instance, there was high certainty evidence (for prognosis and prediction) available for 30-day mortality using cardiac troponins at each time point. However, the evidence for 1-year major adverse cardiac events varied from very low to low depending on the time point of measurement.
- There was a significant gradient in the certainty of evidence across the three scopes of biomarker measurement applications (prognosis, prediction, and biomarker-enhanced management). Evidence on biomarker-enhanced management was extremely scarce. While there was very low-quality evidence suggesting improvement in specific outcomes with secondary prophylaxis in patients with perioperative myocardial injury, there were no data on the impact of a systematic troponin surveillance program on outcomes of patients who did not undergo troponin measurement.
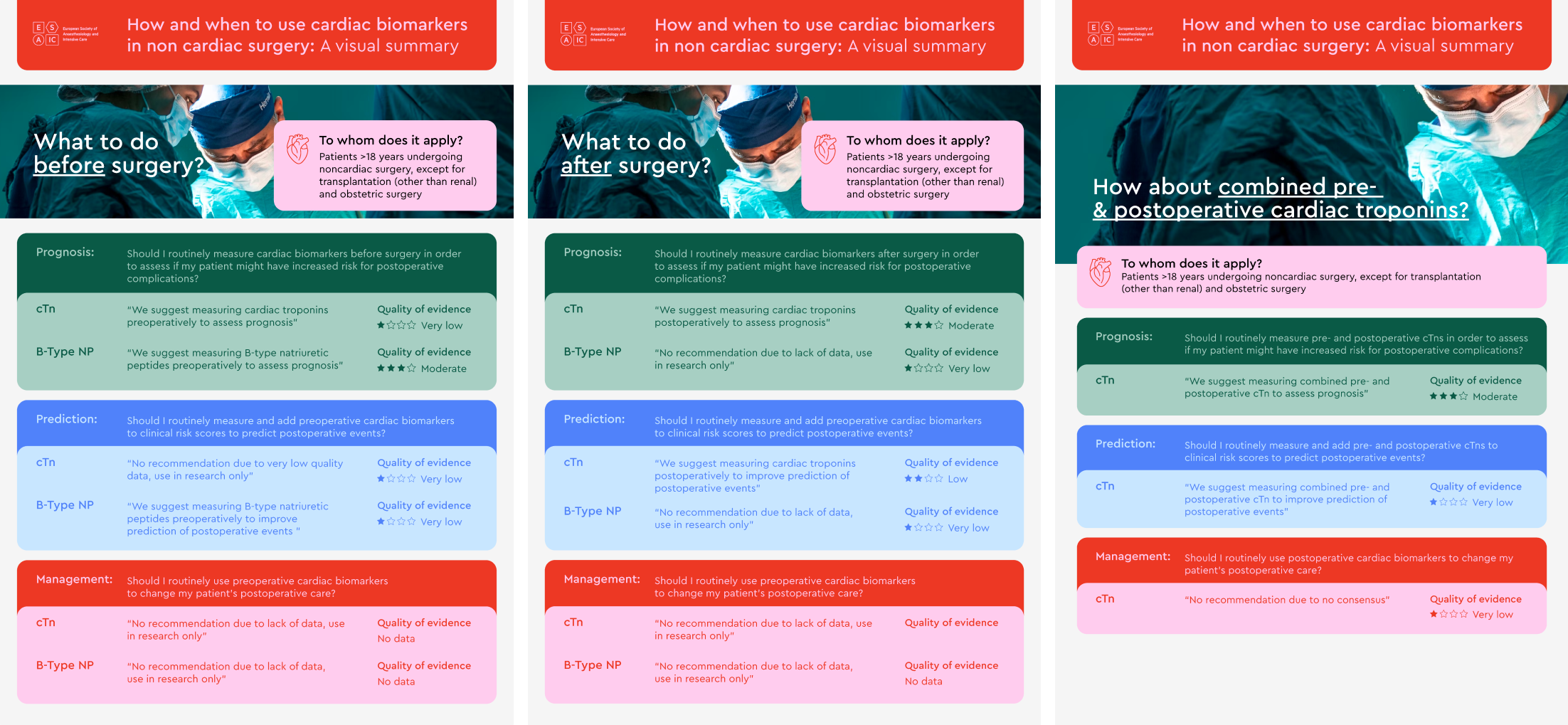
Regarding the use of biomarkers for prognosis, the task force issued weak recommendations for preoperative cardiac troponin (weak in favour, very low certainty), combined pre- and postoperative cardiac troponin (weak in favour, moderate certainty), postoperative troponin (weak in favour, moderate certainty), and preoperative B-type natriuretic peptides (weak in favour, moderate certainty). The guidelines suggested that routine measurement of these cardiac biomarkers may be used to assess the risk of adverse outcomes and provide better information to patients before surgery.
For the use of biomarkers in prediction, the panellists issued weak recommendations for combined pre- and postoperative cardiac troponin (weak in favour, very low certainty), postoperative troponin (weak in favour, low certainty), and preoperative B-type natriuretic peptides (weak in favour, very low certainty). The guidelines suggested that routine measurement of these biomarkers may be considered to predict specific postoperative outcomes.
Regarding biomarker-enhanced management, the task force found very low certainty or lack of evidence for the systematic measurement of biomarkers to guide interventions and improve outcomes in at-risk patients. Therefore, the task force suggested limiting the use of preoperative cardiac troponin, postoperative troponin, and preoperative B-type natriuretic peptide for this purpose to research contexts only. The panellists agreed that combined pre- and postoperative troponin measurement helps differentiate between acute myocardial injury and chronic troponin elevations, making it preferable to isolated postoperative troponin measurement. However, due to strong differences of opinion among the panellists regarding systematic troponin surveillance, a consensus was not reached, and no recommendation was issued. In the accompanying clinical practice statement, the task force emphasized that “the combined measurement of pre- and postoperative cardiac troponins can aid in diagnosing asymptomatic myocardial injury/infarction and other treatable conditions (e.g., heart failure, arrhythmias, pulmonary embolism, sepsis) since increased levels may indicate the presence of these complications.” Furthermore, the panellists considered it desirable for centres already conducting pre- and postoperative cardiac troponin surveillance and corresponding interventions to integrate such a program within a clinical research framework.
During the preparation of the current focused guidelines by the ESAIC (LINK), the European Society of Cardiology (ESC) updated the 2014 guidelines on cardiovascular risk assessment and management of patients undergoing noncardiac surgery. The ESC guidelines, published in August 2022, strongly recommended perioperative troponin surveillance (class I) for patients with cardiovascular risk factors or those over 65 years of age undergoing intermediate or high-risk procedures. They recommended using a high-sensitivity assay for troponin surveillance, starting preoperatively and continuing up to 48 hours after surgery. For preoperative B-type natriuretic peptide, the recommendation was classified as IIa (“should be considered”) in the same population.
Readers may notice an inconsistency between the strong recommendation for perioperative troponin surveillance and associated interventions issued by the ESC and the weak recommendations specific to prognosis and prediction for perioperative troponin measurement issued by the ESAIC. How did these two panels reach apparently different conclusions? What are the similarities?
Both panels acknowledge the prognostic significance of silent myocardial injury and recognize that a perioperative surveillance program can assist in diagnosing asymptomatic myocardial injury, myocardial infarction, and potentially other treatable conditions (e.g., heart failure, arrhythmias, pulmonary embolism, sepsis). However, the two panels employed different methodologies, which may partly explain why they arrived at similar directions with varying intensities.
Firstly, the ESAIC task force defined critical outcomes of interest in advance through the Delphi process, resulting in 12 critical outcomes. While there was high certainty of evidence for some of these outcomes, data were lacking for many others. The prior definition of outcomes raised awareness of significant knowledge gaps.
Secondly, the ESAIC panel differentiated and independently assessed the certainty of evidence for three different applications: prognosis, prediction, and biomarker-enhanced management. This approach highlighted the scarcity of data on biomarker-enhanced management. ESAIC panellists considered that data suggested some benefit from secondary prophylaxis, such as aspirin and statins, in patients with detected myocardial injury compared to non-treatment. However, there was no data investigating outcomes among patients receiving troponin surveillance versus those who did not. Additionally, the lack of information on potential adverse effects prevented the evaluation of the clinical risk-benefit balance, which, in turn, hindered any assessment of cost-effectiveness. Considering these factors, the ESAIC panel could not recommend systematic perioperative troponin surveillance and troponin-enhanced management.
In conclusion, both guidelines recognize the prognostic significance of elevated cardiac biomarkers and perioperative myocardial injury. The ESC guidelines focus on the positive aspects and advocate for proactive measures. On the other hand, the ESAIC guidelines take a more cautious approach, emphasizing the knowledge gaps. Hopefully, new studies will soon shed light on the complete picture.
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter”]