ESAIC News
Is neuromuscular monitoring the wave of the future in general anaesthesia?
To monitor or not to monitor – that is the question at the center of the debate over quantitative neuromuscular monitoring, going on at Euroanaesthesia 2024.
Neuromuscular blocking agents (NMBAs) are used to improve airway management and facilitate intubation during general anaesthesia. However, results from large retrospective studies have revealed a link between the use of NMBAs and relaxant-associated postoperative complications,1 which were shown to occur despite adequate reversal with acetylcholinesterase inhibitors or encapsulating agents. With the recent expiration of its patent, sugammadex has become increasingly available in generic formulations at hospitals across Europe, raising new questions about the practices related to the reversal of neuromuscular block in general anaesthesia and the methods for preventing adverse events.
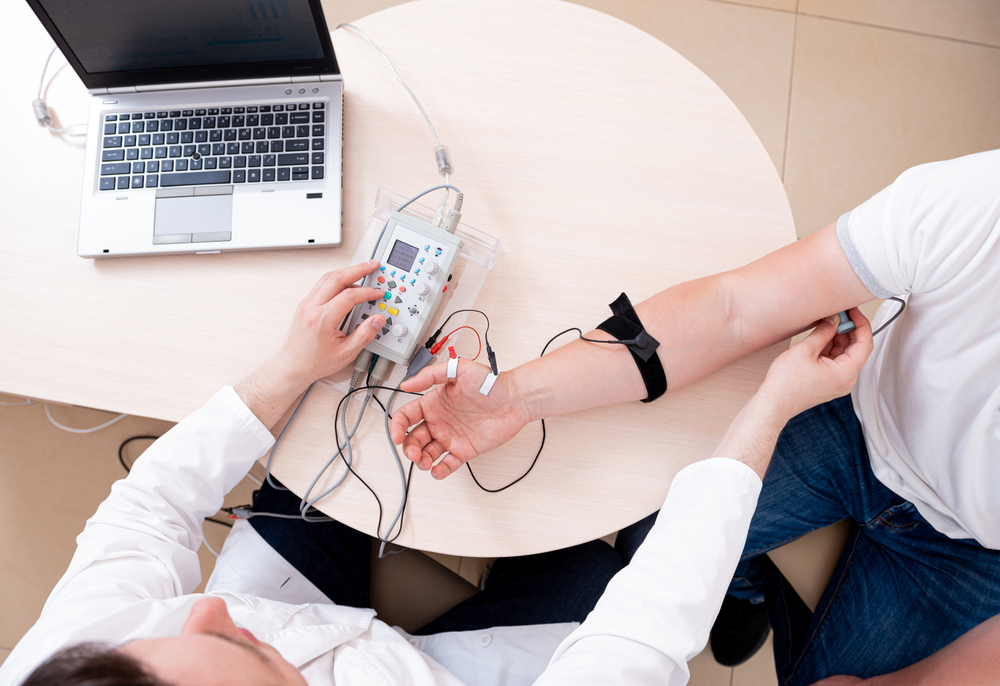
To address the major risks associated with NMBAs, including residual paralysis and postoperative pulmonary complications, ESAIC and the American Society of Anaesthesiologists (ASA) have issued guidelines2,3 that recommend quantitative neuromuscular monitoring, with the use of devices that measure the depth of muscle relaxation during the intubation process. According to these consensus statements, quantitative neuromuscular monitoring is the only reliable method to ensure adequate recovery from the adverse effects of NMBAs in the postoperative period. Nevertheless, anaesthesiologists may find it easier to cling to old habits, such as reliance on the subjective evaluation of clinical signs to confirm recovery from neuromuscular block. Data preceding the ESAIC guidelines showed that less than one-fifth of patients across Europe underwent quantitative neuromuscular monitoring during general anaesthesia.1
While the ESAIC and ASA guidelines have identified the switch to routine quantitative neuromuscular monitoring as the most crucial step toward improving patient outcomes, promoting the widespread use of this method is a long-term strategy. The implementation of quantitative monitoring in clinical practice must break down barriers such as the lack of institutional standards and protocols, time constraints, suboptimal clinician training, and the limited availability of quantitative train-of-four (TOF) monitors in clinical practice. Misconceptions about the pharmacokinetics of NMBAs and residual block may constitute another roadblock in the way of optimising the perioperative management of neuromuscular blockade.
The lack of reliable information about the role and efficacy of neuromuscular monitoring during general anaesthesia persists in the European practice of anaesthesiology, despite the recent recommendations. In some clinical settings, quantitative neuromonitoring is considered unnecessary when sugammadex is used to reverse the effects of aminosteroidal agents such as rocuronium or vecuronium. However, anytime a NMBA is administered, neuromuscular monitoring should be used to guide administration and adequately reverse the effects of neuromuscular blockade, according to the recent guidelines. Quantitative neuromuscular may also be perceived as expensive, difficult to interpret, and likely to fail during surgical procedures.
While clinical signs have traditionally been used to confirm adequate reversal of neuromuscular blockade, these are unreliable in unconscious patients. Instead, ESAIC recommends the use of ulnar nerve stimulation and quantitative neuromuscular monitoring at the adductor pollicis muscle to exclude residual paralysis. Moreover, monitoring of neuromuscular blockade should be continued until a TOF ratio of more than 0.9 has been attained. The guidelines emphasise the limitations of qualitative devices and clinical assessment in distinguishing between adequate recovery and minimal levels of residual blockade, and the significance of distinguishing between deep, moderate, shallow, and minimal levels of neuromuscular blockade.
As long as some clinicians remain skeptical about the role of intraoperative monitoring in reducing the rates of NMBA-related complications, the controversy is alive and well. During a pro-con debate on Monday, Prof. Thomas Fuchs-Buder, MD, and his co-speakers will address common misconceptions about the use of neuromuscular monitors and reversal agents in the practice of anaesthesiology, as well as the importance of educating clinicians about quantitative monitoring. Fuchs-Buder, a professor of anaesthesiology at the University of Lorraine, Centre Hospitalier Universitaire de Nancy, Hôpitaux de Brabois, in France, is a co-author of the ESAIC guidelines and a lead researcher in the field of neuromuscular monitoring during anaesthesia.
References:
- Kirmeier E, Eriksson LI, Lewald H, et al; POPULAR Contributors. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med 2019;7(2):129-140.
- Fuchs-Buder T, Romero CS, Lewald H, et al. Peri-operative management of neuromuscular blockade: A guideline from the European Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol 2023;40(2):82-94.
- Thilen SR, Weigel WA, Todd MM, et al. 2023 American Society of Anesthesiologists Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade. Anesthesiology 2023;138(1):13-41.










