Newsletter 2023
Newsletter July 2023: New version of the ESAIC guidelines on severe perioperative bleeding management
Severe bleeding in major surgery is an emergency. Guidance for avoiding and controlling bleeding and anaemia and in reducing the need for allogeneic blood transfusions improves patient outcomes and makes our lives as clinicians easier. Accordingly, there was, and still is, a need for clinical guidelines.
About 15 years ago, direct oral anticoagulants became available. There was broader use of viscoelastic haemostatic assays (VHAs) and bedside platelet function analysers. Furthermore, insights from scientific evidence were evolving. Therefore, the ESAIC nominated a task force and defined the scope: to provide a set of recommendations for the multi-modal care for the management of severe perioperative bleeding in various clinical scenarios. Ten years ago, this task was accomplished, and our bleeding guidelines were published in Eur J Anaesthesiol [^1].
Anaesthesiology is a rapidly evolving medical field. The concept of Patient Blood Management (PBM) has been increasingly acknowledged, and more attention has been paid to the appropriate use of blood products. Additionally, new anticoagulant antidotes have become available. These aspects were captured in our first guidelines update published in 2017 [^2].
Regular updates are required for all our evidence-based guidelines. The ESAIC strategy is to update guidelines regularly every 3-5 years. Consequently, ESAIC re-nominated the task force in 2020 to start preparing the second update because there is still a need for guidance in basically all clinical fields where severe bleeding may be encountered. There were new challenges in haemostasis management during the COVID pandemic, some medications were withdrawn from the market, while others entered the market. Revised management is now detailed in the second guidelines update [^3].
Main Results
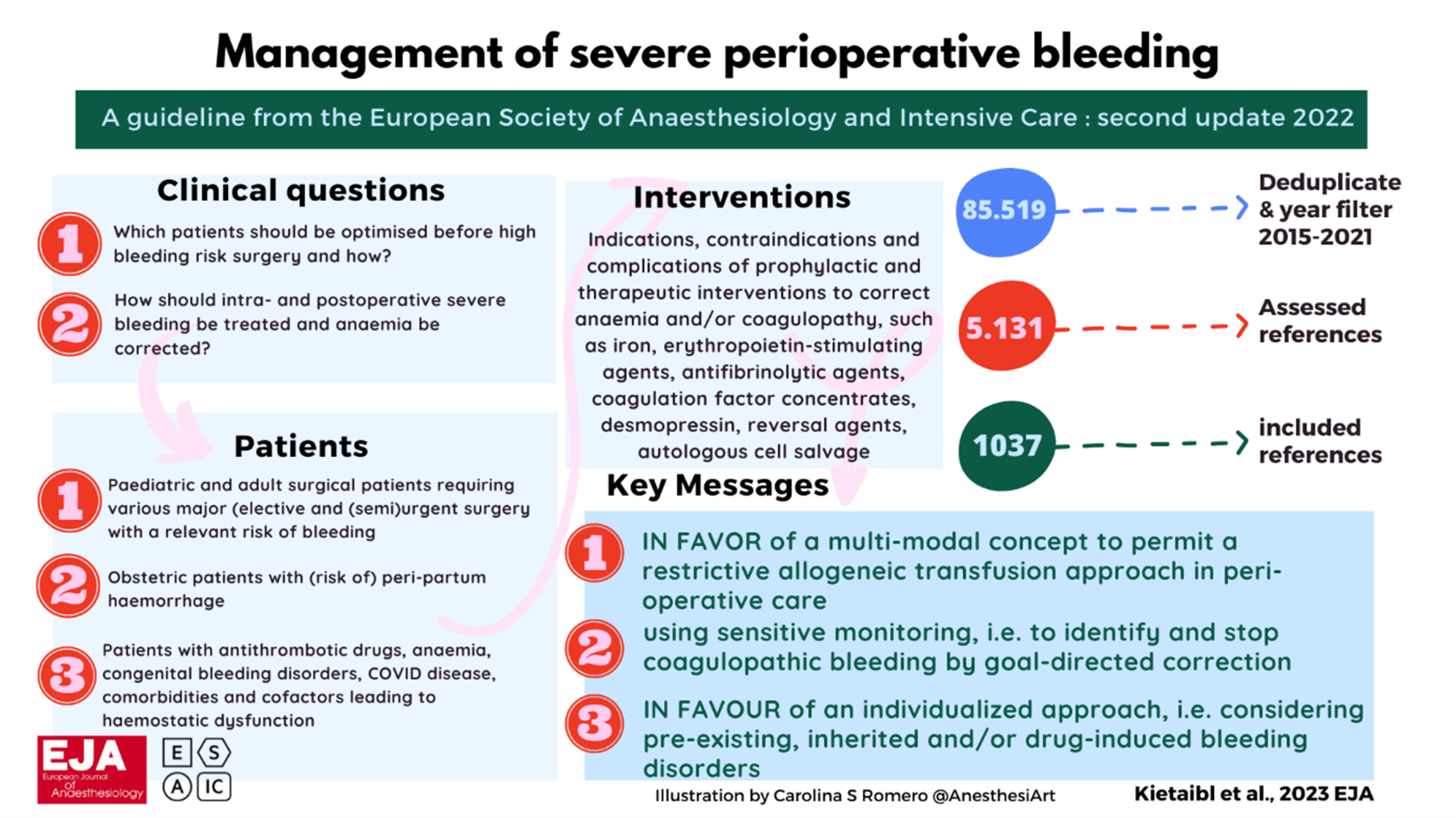
We focused on 2 clinical questions:
- Which patients should be optimised BEFORE surgery and how?
- How should INTRA- and POSTOP bleeding be treated, and anaemia be corrected?
The foundation of our guidance is the systematic literature search covering 2015 to 2021, which retrieved over 85,000 articles, more than 1,000 of which are included in the reference list. In addition to the recommendations derived from the systematic literature search, we reconfirmed guidance from the 2017 version and clearly presented those that are still relevant.
There is a lot of content within the second update. Overall, guidance is summarised in 253 sentences. There are many new recommendations, suggestions, and statements. Much more detail can be found within specific chapters on bleeding management in visceral, orthopedic, and pediatric surgery, and also regarding anaemia management after surgery. Among the task force, strong consensus of 97% and consensus of 3% was achieved in our Delphi process: this guideline represents a strong opinion. For those sentences with consensus only (but not strong consensus), we explained in the text how we clarified these issues. For example, we could not define a target value for factor XIII supplementation in two 2C suggestions; we, therefore, decided not to include any percentage of factor XIII activity at all.
Some GRADEings changed: specifically, 13 GRADEs increased due to a better body of evidence over the previous years; 6 GRADEs appear to have decreased, but actually, the content of the recommendation has been enriched. There are also some content changes, e.g., perioperative bridging of vitamin K antagonists with heparin is less prevalent.
While new or changed content is important for a guidelines update, continuity is also crucial. The second update of our ESAIC guidelines on the management of severe perioperative bleeding points in the same direction as previously:
- In high bleeding risk surgery:
- Pre-existing anaemia should be detected and corrected pre-operatively to increase the patients’ tolerance to perioperative surgical and coagulopathic blood loss, as well as to avoid allogeneic blood transfusions.
- Pre-existing inherited, drug-induced and/or acquired bleeding disorders, including coagulopathy in critical illness, should be detected and corrected pre-operatively to reduce perioperative blood loss and allogeneic blood product requirements.
- Autologous cell salvage and antifibrinolytic prophylaxis should be exploited whenever possible. Body temperature, homeostasis, and tissue perfusion should be monitored and kept normal.
- Surgical bleeding events should be stopped by surgical measures.
- Acquired coagulopathic bleeding events should be stopped by individualised correction of the actual pathomechanism(s) of bleeding by antifibrinolytic and/or prohaemostatic drugs, preferably potent virus-inactivated coagulation factor concentrates.
In fact, the ESAIC guideline is a credo for an individualised management approach:
- Consider patient- and surgery-specific risks.
- Prevent progression of some bleeding to severe/massive bleeding.
- Correct coagulopathy before it becomes massive.
- Check the dynamics of the clinical situation and monitor appropriate lab data.
- Calculate needs and dosages according to your internal hospital algorithm.
- Consider the appropriate sequence of prohaemostatic medications.
- Re-check and re-monitor clinical data and appropriate lab data.
In contrast, a non-individualised ratio-based management approach is only suggested in an early treatment phase of uncontrolled elective surgery bleeding with a ratio of ≥1:1 of plasma:red blood cell (RBC) in massive transfusion (>6-10 RBC).
Main Unexpected Results
There were no unexpected results. Our suggestion to use prothrombin complex concentrate (PCC) instead of andexanet alpha in elective surgery bleeding related to direct factor Xa inhibitors may appear contradictory to the trauma setting. However, licensing issues and recent evidence on efficacy, monitoring, and safety in these clinical scenarios explain the discrepancy.
Main Unexpected Obstacles
Overall, the guideline methodology for this project was similar to other ESAIC guidelines. During the COVID pandemic, however, communication among the task force was via email, virtual, and hybrid meetings. We perceive this approach as inferior to face-to-face meetings and discussions.
Patient Benefit
Also unchanged is the focus our ESAIC guidelines have on patient safety. Guidelines adherence will result in PBM implementation [^4], including avoidance of RBC transfusion when anaemia correction is recommended instead, avoidance of plasma transfusion when PCC is recommended instead, bleeding control with VHA-guided supplementation in acquired coagulation factor deficiencies. In fact, our ESAIC guidelines are the European perioperative PBM guidelines. Patient benefit from guidance can only be expected if evidence-based tips from recommendations and suggestions are implemented into daily clinical practice.
Feasibility of Implementation Across Europe
Initiating guidelines preparation with two highly relevant clinical questions and considering bleeding scenarios in literally all clinical fields should per se facilitate guidelines implementation. Task force members are not desk-researchers but clinicians. Therefore, the content of the ESAIC guidelines is suitable for the front line. According to the availability of resources, not all aspects of the guidelines can be implemented completely across Europe.
Writing guidelines is a difficult task, but implementing guidelines, especially multi-modal interdisciplinary content, is much more difficult. So the big challenge is on your side, dear ESAIC members.
Here are some ideas for implementation at a departmental level:
- General knowledge transfer: use internal hospital education and team trainings on individualised management of anaemia, bleeding, hypovolaemia, transfusions.
- Enhanced: create a culture/microclimate of applied PBM.
- Further enhanced: involve your surgeons, internal medicine and lab physicians, and family doctors for a harmonised strategy.
- Translate the ESAIC guidelines into your infrastructure: define within your internal hospital, surgery-specific algorithms for the management of anaemia, coagulopathy, and for your allogeneic transfusion strategy.
- Enhanced: import the algorithms into your electronic hospital information systems.
- Track costs to report cost-effectiveness to your hospital administrators for further support in infrastructures such as appropriate lab tests and/or prohaemostatic medications.
- Inform your patients and laypeople about your excellence in ESAIC guidelines implementation.
- Enhanced: translate guidelines into patients’ language [^5].
- Further enhanced: include guidelines adherence as a national quality indicator.
- Do implementation research and publish it [^6].
There is still no recipe for guidelines implementation. We hope that we may further assist you in bringing evidence to the bedside and in detecting/stopping non-evidence by preparing aids at hand. Our application for smartphones on the ESAIC/ERSA guidelines on regional anaesthesia in patients on antithrombotic drugs [^7] will shortly include all the content of our 19 recommendations and 4 reconfirmed statements.
References
- Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Eur J Anaesthesiol 2013;30:270-382
- Kozek-Langenecker SA, Ahmed AB, Afshari A, et al. Eur J Anaesthesiol 2017;34:332-395
- Kietaibl S, Ahmed A, Afshari A, et al. Eur J Anaesthesiol 2023;40:226-304
- World Health Organization 2021. ISBN 978-92-4-003574-4 (electronic version)
- https://www.youtube.com/watch?v=cjVYBoqj2sM
- Kietaibl S. Eur J Anaesthesiol 2022;39:1-3
- Application for smartphones from Gesellschaft für Schmerztherapie und Anästhesiologie
- (search app store or google play for: regional anaesthesia)
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter”]