Newsletter 2023
Newsletter July 2023: Update of the ESAIC guideline on the prevention and management of postoperative delirium
Claudia Spies, on behalf of the ESAIC Task Force and the ESAIC Advisory Board
This project was motivated by the need to update the 2017 guideline on the prevention of postoperative delirium (POD) published by the European Society of Anaesthesiology (ESA). A comprehensive literature search in 2020 revealed a significant number of references, prompting a thorough review and analysis of the latest evidence.
Six working groups focused on various aspects of POD, conducting specific literature searches and generating prioritized questions and recommendations. Defining the outcome of POD posed an unexpected obstacle, leading to the establishment of a new screening algorithm. Pre-post study designs faced challenges in outcome assessment, resulting in a reduction of included studies.
The main results emphasized a team approach and the implementation of non-pharmacologic preventive measures. Pre-operative risk assessment and multi-component interventions were recommended for high-risk patients. Implementation across Europe could benefit from best practice examples and lighthouse projects already in place.
Ultimately, the project aimed to improve patient outcomes by implementing transformational pathways for POD prevention, monitoring, and treatment. The evidence supports the effectiveness of preventive strategies, underscoring the importance of a collaborative approach and early intervention.
We interviewed the Task Force and the ESAIC Advisory Board about what triggered the revision and the challenges they face, and we are sharing those insights with our readership on this article.
What motivated you to undertake this project?
The update of the 2017 published ESA guideline on the prevention of postoperative delirium (POD) was a planned update five years after the completion of the previous literature search. The limit of the previous literature search was March 2015. In November 2020, a comprehensive literature search using the identical search terms as the previous guideline revealed nearly 2,300 references in PubMed, of which over 1,200 were potentially relevant for the update. A follow-up in February 2022 identified a further 500 potentially relevant references in PubMed.
Main PICO:
The ‘Key questions’ from the 2017 guideline were transformed into PICO questions, and six working groups (basic science, risk factors, pharmacologic prevention, non-pharmacologic prevention, neuromonitoring, treatment & outcome) conducted specific literature searches for individual PICO questions, using the broad literature search when necessary. The six working groups generated 20 prioritised PICO questions, leading to 13 recommendations. All PICO questions deal with POD in adult patients undergoing anaesthesia and surgery.
What were the main unexpected obstacles and barriers?
The primary unexpected obstacle encountered during literature screening was defining the outcome, POD. As delirium displays a fluctuating course throughout the day, a valid diagnosis requires multiple screenings daily. However, several studies screened once per day, some not even daily. The working group agreed on a minimal screening algorithm, requiring POD to be measured with a validated screening tool at least once per day for at least three days starting in the recovery room or post-anaesthesia care unit on the day of surgery or, at the latest, on postoperative day 1. This definition increased confidence in single study outcomes but necessitated re-evaluating all existing systematic reviews and meta-analyses on POD prevention, as many included single studies that did not fulfil this new POD gold standard definition. The POD working group hopes to set a new standard for POD screening in future studies and daily clinical practice with POD assessments in every shift (so 2-3 times per day) for at least the first three postoperative days.
Pre-/post-study designs are useful for evaluating sequential interventions. As randomisation is often not feasible in multi-component interventions, pre-post studies can provide essential evidence. However, assessing the outcome was again challenging. POD assessment often differed between control and intervention periods, and only the latter was prospectively done. Excluding pre-post studies due to methodological concerns reduced the number of included studies.
What were the main results and ideas for implementation emerging from this work?
A transformational culture is required to implement POD prevention, monitoring, and treatment strategies. This update further emphasises the need for a team approach, where multiple perioperative disciplines work together and initiate a set of non-pharmacologic preventive measures. The pre-operative risk assessment should begin at the first contact with the patient allowing prehabilitation and pre-operative optimisation strategies when indicated. Patients at increased risk for POD benefit from multi-component interventions, which may include bundles with general measures or more tailored interventions based on individual risk assessments. Implementation is feasible on the ward, at hospital level, and even pre-clinically, including ambulatory structures and pre-hospital ambulatory medicine.
Feasibility of implementation across Europe and ideas to tackle the obstacles: Several European countries have already implemented delirium prevention programmes in single hospitals, with best practice examples available. This updated guideline aims to accelerate the implementation of such lighthouse projects into multi-professional, interdisciplinary, and intersectoral basic and regular care.
Do Patients benefit from the new evidence, and if yes, how?
Currently, there is clear evidence that preventive strategies are beneficial. Therefore, patients benefit from transformational pathways (see Figure 1) that evaluate risk factors, optimise patients’ predisposing factors, avoid and minimise surgery- and anaesthesia-related precipitating risk factors, and – if POD cannot be prevented – allow early detection and treatment.
References
Aldecoa, César; Bettelli, Gabriella; Bilotta, Federico; Sanders, Robert D.; Audisio, Riccardo; Borozdina, Anastasia; Cherubini, Antonio; Jones, Christina; Kehlet, Henrik; MacLullich, Alasdair; Radtke, Finn; Riese, Florian; Slooter, Arjen J.C.; Veyckemans, Francis; Kramer, Sylvia; Neuner, Bruno; Weiss, Bjoern; Spies, Claudia D.. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. European Journal of Anaesthesiology 34(4):p 192-214, April 2017. | DOI: 10.1097/EJA.0000000000000594
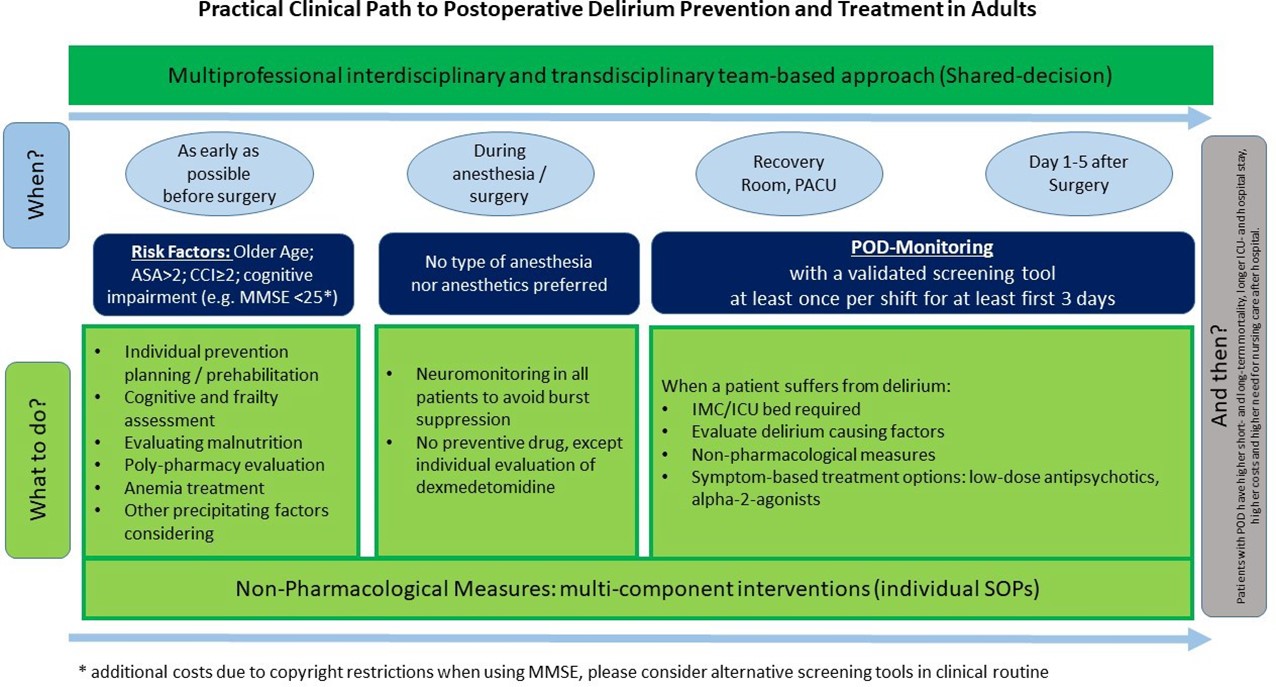
Figure 1: Practical Clinical Path to Postoperative Delirium Prevention and Treatment in Adults
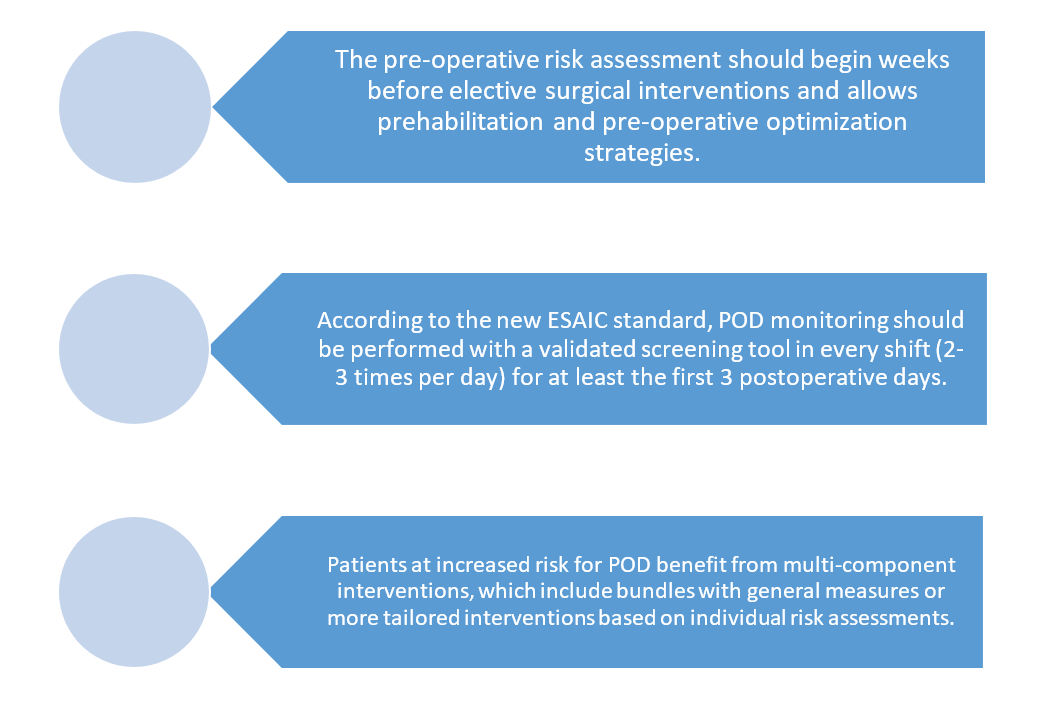
Figure 2: Take Home Messages
[maxbutton id=”1″ url=”https://www.esaic.org/newsletter/” text=”Read the Newsletter”]










