Newsletter 2023
Newsletter September 2023: Improving Patient Safety and Quality with a patient-centred approach in Anaesthesia care - The Safe Brain Initiative Approach
Author:
Basak Ceyda Meco, Joana Berger-Estilita, Karina Jakobsen, Finn M. Radtke
‘How are our patients doing in the postoperative period?’ This query should constitute a vital inquiry within the realm of safety metrics.
Anaesthesiology has been a pioneering discipline in patient safety for decades, demonstrating sustained and progressive efforts in propagating fundamental standards and guidelines relevant to the patient safety domain.(1) Moreover, in recent decades, healthcare systems have undergone a significant shift in recognising the significance of patients’ perspectives and feedback as vital to ensuring that medical services are of high quality and delivered equitably and safely.(2) Today, integrating patient feedback and patient-reported outcome measures (PROMs) has gained significant weight and a critical role in the anaesthesia practice as a central instrument in ensuring secure and high-quality perioperative care. Growing evidence supports that integrating patients’ feedback and PROMs into the routine care of patients improves safety, quality, and shared decision-making.(3-5) However, in the ever-changing healthcare areas, healthcare professionals and hospital administrators face increasingly significant difficulty in collecting organised and systematic feedback on patient reporter outcome measures (PROMs).(6) This lack of systematic feedback systems for PROMs and complications is a pressing concern for anesthesiologists.
PROMs are standardised questionnaires that collect information on health outcomes directly from patients, including symptoms and functional outcomes following interventions such as anaesthesia and surgery. They offer a means to gauge patient’s perspectives on their individual outcomes.(7) Critical perioperative PROMs can be defined as postoperative pain, postoperative nausea and vomiting, thirst, stress-anxiety, well-being, and odynophagia. In this context, postoperative delirium and neurocognitive disorders also necessitate attention.
The implementation and utilisation of validated tools to measure PROMs have emerged as an accelerator for quality improvement in perioperative healthcare. As a pivotal element of precision care, these tools facilitate the direct gathering of comprehensive patient information, thereby enabling personalised patient-centred care.(8)
The Safe Brain Initiative (SBI) project aims to address this issue through a systematic approach to generate and use real-world data to monitor and improve PROMs and to prevent and reduce postoperative delirium and neurocognitive disorders in the perioperative period.(9) It represents a proactive effort to bridge the feedback gap by assessing systematically and repetitively patients’ results. Through the systematic follow-up of PROMs, this approach aims to strengthen perioperative patient care, optimise treatments and promote a safer patient-centred perioperative environment.
The focus of the SBI approach can be defined as visualising and achieving the best PROMs, accomplishing an effective and sustainable, patient-centred OR management, and targeting higher patient and staff satisfaction with the provided care.
The Safe Brain Initiative is an international, non-profit, research-based solution for monitoring and improving the PROMs mentioned above and avoiding and decreasing postoperative delirium and neurocognitive disorders in the perioperative context.
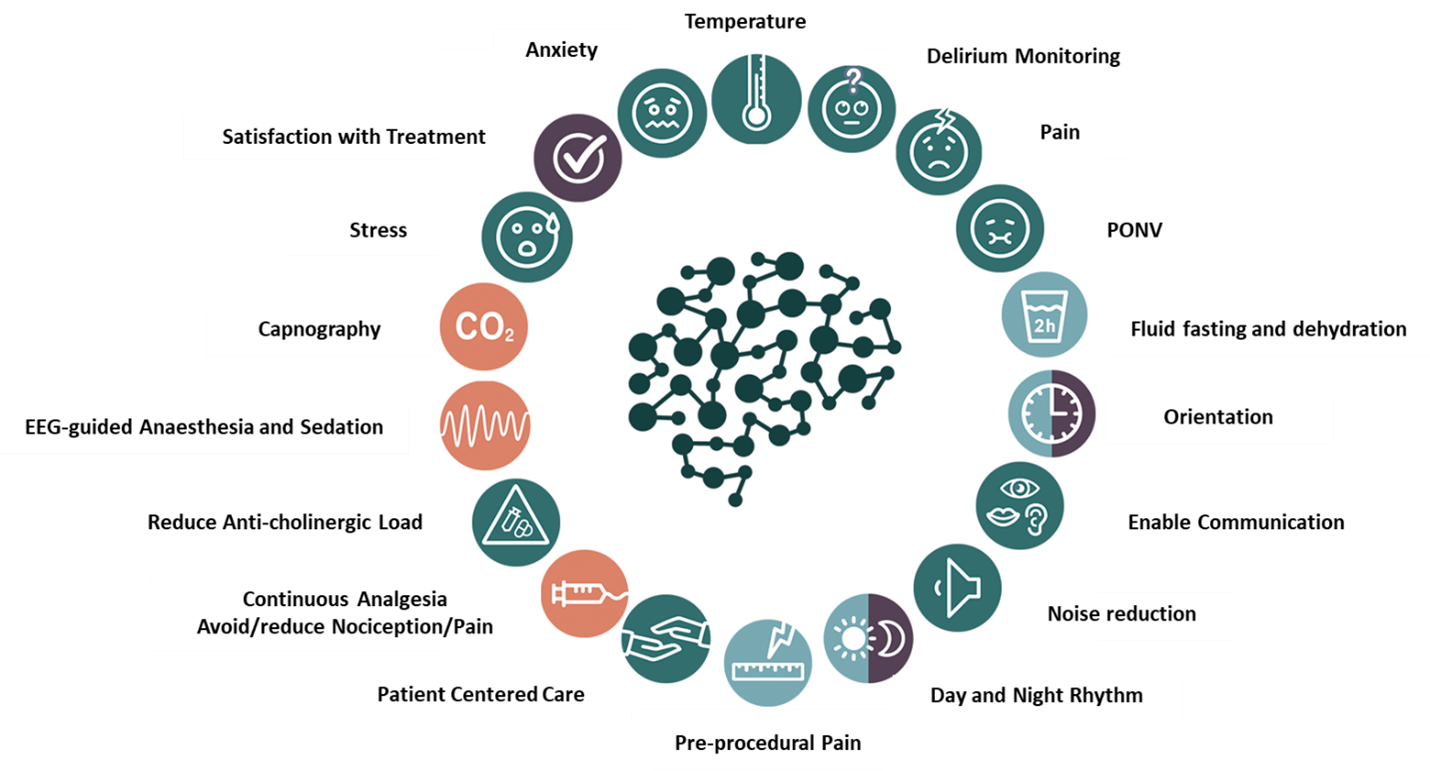
With its current 18 non-invasive core recommendations (Figure 1), the SBI aims to detect and prevent adverse PROMs, including postoperative delirium and neurocognitive disorders, postoperative nausea and vomiting, perioperative pain, perioperative stress-anxiety, and patient discomfort. These recommendations are derived from international guidelines or expert consensus, with the primary objective of enhancing the patient’s perioperative experience while reducing the iatrogenic load of negative precipitating factors on patients’ postoperative outcomes. By incorporating these recommendations and corresponding non-invasive interventions into routine practice, healthcare providers can improve the safety and quality standards within the perioperative setting. The main focus of the SBI project is achieving the best PROMs with effective, efficient, and sustainable patient-centred perioperative management. Furthermore, patient and staff satisfaction with the provided care is also a primary aim of the project.
The Safe Brain Initiative also strives to evolve into a research-based comprehensive solution for monitoring, preventing, and managing postoperative delirium and neurocognitive disorders within the perioperative context.
Postoperative Delirium and Neurocognitive disorders represent significant adverse events within the perioperative period and a large-scale public health issue with substantial costs, rivalling costs associated with cardiovascular disease and diabetes. POD episodes significantly increase the length of hospital stay, increasing patient hospitalisation costs and limiting the availability of beds to receive more patients. In that regard, the importance of the SBI approach already automatically highlights itself as fulfilling and enhancing the aims and vision of anaesthesiologists.
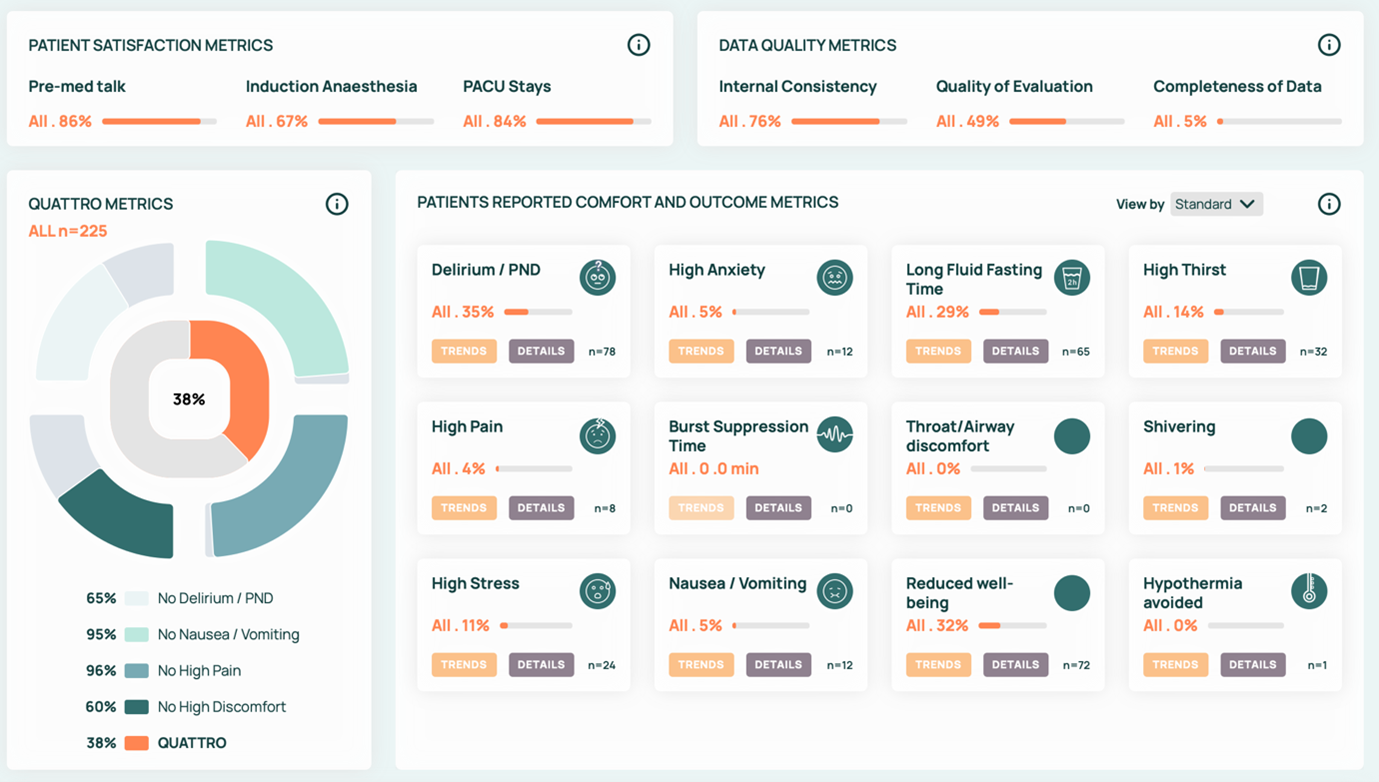
The Safe Brain Initiative also represents a comprehensive framework for implementing and operationalising real-world data in the perioperative setting. With its data-driven dashboard solution, the SBI offers a systematic and active feedback tool to all participants involved (Figure 2).
Patient-centred strategies, such as the Safe Brain Initiative (SBI), are cost-effective and serve as essential instruments for enhancing PROMs through the engagement of patients in shaping their medical trajectories.(10)
In conclusion, the SBI project aims to develop and improve an international multicenter web-based, guideline-supported, and anaesthesia society-endorsed solution for teaching, evaluating, displaying, and optimising PROMs and adverse cognitive outcomes in the perioperative setting.
The European Society of Anaesthesiology and Intensive Care (ESAIC) has recently endorsed the Safe Brain Initiative by acknowledging it as a Research Group within the Society in recognition of its substantial value and prospective impact. Additional details and insights about the project can be retrieved from the Safe Brain Initiative’s official website: safebraininitiative.com.
We invite all European Hospitals to participate in this Safe Brain Initiative project for international collaboration to create a patient-centred, PROM-focused precision anaesthesia care practice and foster beneficial changes in perioperative care.
References
- Harbell MW, Methangkool E. Patient safety education in anaesthesia: current state and future directions.Curr Opin in Anesthesiol. 2021;34:720-725
- Churruca K, Pomare C, Ellis LA et al. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues Health Expectations 2021; 24: 1015-1024.
- Okuyama JHH, Galvao TF, Silva MT. Healthcare professional’s perception of patient safety measured by the hospital survey on patient safety culture: a systematic review and meta-analysis. Sci World J 2018;2018:11.
- Docter S, Fathalla Z, Lukacs MJ, et al. Interpreting patient-reported outcome measures in orthopaedic surgery: a systematic review. J Bone Joint Surg Am 2021;103:185–90.
- Makhni EC. Meaningful clinical applications of patient-reported outcome measures in orthopaedics. J Bone Joint Surg Am 2021;103:84–91.).
- Anderson M, Pitchforth E, Vallance-Owen A, et al. Misconceiving patient-reported outcome measures (PROMs) as primarily a reporting requirement rather than a quality improvement tool: perceptions of independent healthcare sector stakeholders in the UK. J Patient Rep Outcomes. Sep 23 2022;6(1):101. doi:10.1186/s41687-022-00511-5.
- Weldring T, Smith SM. Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv Insights. 2013;6:61-8. doi:10.4137/HSI.S11093///Kingsley C, Patel S. Patient-reported outcome and experience measures. Bja Education. 2017;17(4):137-144.
- Warnakulasueiya SR, Patel RC, Singleton GF et al. Patient-reported outcomes for ambulatory surgery. Curr opin Anaesthesiol 2020; 33:768-773, 4.
- Safe Brain Initiative. Accessed 8th June 2023, https://safebraininitiative.com
- Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. Jun 19 2014;14:271. doi:10.1186/1472-6963-14-271
Figure 1: The 18 SBI Core recommendations
- Delirium monitoring: Implement measures to monitor and detect delirium in the perioperative period.
- Preoperative Pain: Address and treat pain before surgery to improve patient experience.
- Stress: Employ strategies to lessen perioperative stress, fostering a more tranquil patient environment.
- Anxiety: Recognise, address and reduce perioperative anxiety in patients through appropriate interventions and support.
- Oral Fluid Fasting Duration: Curtail unnecessary pre and post-surgery fasting periods.
- Postoperative Nausea and Vomiting (PONV): Implement and fine-tune preventative measures and treatments for nausea and vomiting post-surgery.
- Postoperative Pain: Evaluate and effectively fine-tune preventive and postoperative pain treatment.
- Facilitate Communication: Ascertain that patients bring their dentures, hearing aids, and glasses to the Operating Room (OR), Post Anaesthesia Care Unit (PACU), and throughout the perioperative pathway, where applicable. This strategy aids in maintaining orientation and fostering and enhancing patient-centred communication between healthcare professionals and patients, thereby ensuring a transparent and effective exchange of information.
- Patient-Centered Clinical Practice: Emphasise a patient-centred approach where the patient’s preferences, needs, and values are considered and respected.
- Anticholinergic influence: reduce the use and influence of anticholinergic medications on cognitive function where possible.
- EEG Monitoring: Utilise the patient’s brain activity using electroencephalography (EEG) to individualise and fine-tune sedation application and to detect and prevent adverse neurological events.
- Continuous analgesics and nociceptive monitoring: Use continuous analgesia techniques (e.g. remifentanil) and validated nociceptive monitoring to fine-tune and manage nociception/pain during and after surgery.
- Use of Capnography in sedated patients: Implement capnography under sedation to ensure adequate ventilation and detect possible complications immediately.
- Circadian Rhythm: Support the patient’s circadian rhythm and incorporate strategies to support the natural sleep-wake cycle during the perioperative period.
- Patient Satisfaction: Measure and address patient satisfaction to improve the quality of care provided for all relevant perioperative care periods.
- Noise: Minimise noise levels in the perioperative environment to promote a calmer and more comfortable patient and staff atmosphere and interaction.
- Orientation: Minimise any potential impacts on patient orientation resulting from the side effects of perioperative care. Strive to maintain or enhance a patient’s baseline orientation concerning spatial awareness, temporal comprehension, and personal data throughout the perioperative period, except during anaesthesia.
- Temperature: Maintain proper perioperative temperature management to prevent hypothermia or hyperthermia and promote patient comfort.
Figure 2: SBI Dashboard example