Newsletter 2021
Post-mastectomy management of pain and postoperative nausea-vomiting
Letter to editor
Tzima Maria
Trainee Anaesthesiologist
martzi88@yahoo.gr
Mendonça et al1 recently published their work on intra-operative esmolol administration in relation to pain treatment following mastectomy. In their work, as a primary outcome, they assess postoperative pain and as secondary, postoperative nausea and vomiting(PONV), blood pressure, heart rate, Bispectral Index(BIS), use of anaesthetics, analgesic medication and time to emergence differences between a group of patients administered esmolol and a control, normal saline group. Although larger trials are still needed, Watts2 and Gelineau3 have performed similar studies; the first showed that esmolol reduced postoperative pain versus placebo, while the second, in a double-blind manner, concluded that evidence was insufficient, although intraoperative opioid consumption was reduced.
Mendonça et al take profit from esmolol’s action as an antinociceptive, acting in the cingulate cortex and trigeminal nucleus, suppressor of adrenergic and inflammatory response, activator of locus coreleus and inhibitor of sodium and calcium transmission, and thus reducing pain. PONV incidence is decreased due to lower opioid consumption and more stable CVS. Their protocol included a bolus dose of 0,5mg/kg in 10 minutes and a constant infusion rate of 100/mcg/kg/min. The side effects of esmolol were treated with symptomatic medication, atropine 0,01 mg/kg for low heart rate and ephedrine 5mg for low blood pressure. Fentanyl was administered in bolus doses of 50mcg.
 As it is already known that mastectomy is followed by an increased incidence of PONV and neuropathic pain, this study offers information of crucial clinical importance. King et al4 compared opioid free anesthesia versus conventional anaesthesia and found no statistical difference in PONV or postoperative opioid needs, a modest decrease in pain scores was noted though. Dinh et al5 applied an ERAS protocol versus a usual care protocol and noticed reduced opioid needs postoperatively, decreased PONV and pain scores.
As it is already known that mastectomy is followed by an increased incidence of PONV and neuropathic pain, this study offers information of crucial clinical importance. King et al4 compared opioid free anesthesia versus conventional anaesthesia and found no statistical difference in PONV or postoperative opioid needs, a modest decrease in pain scores was noted though. Dinh et al5 applied an ERAS protocol versus a usual care protocol and noticed reduced opioid needs postoperatively, decreased PONV and pain scores.
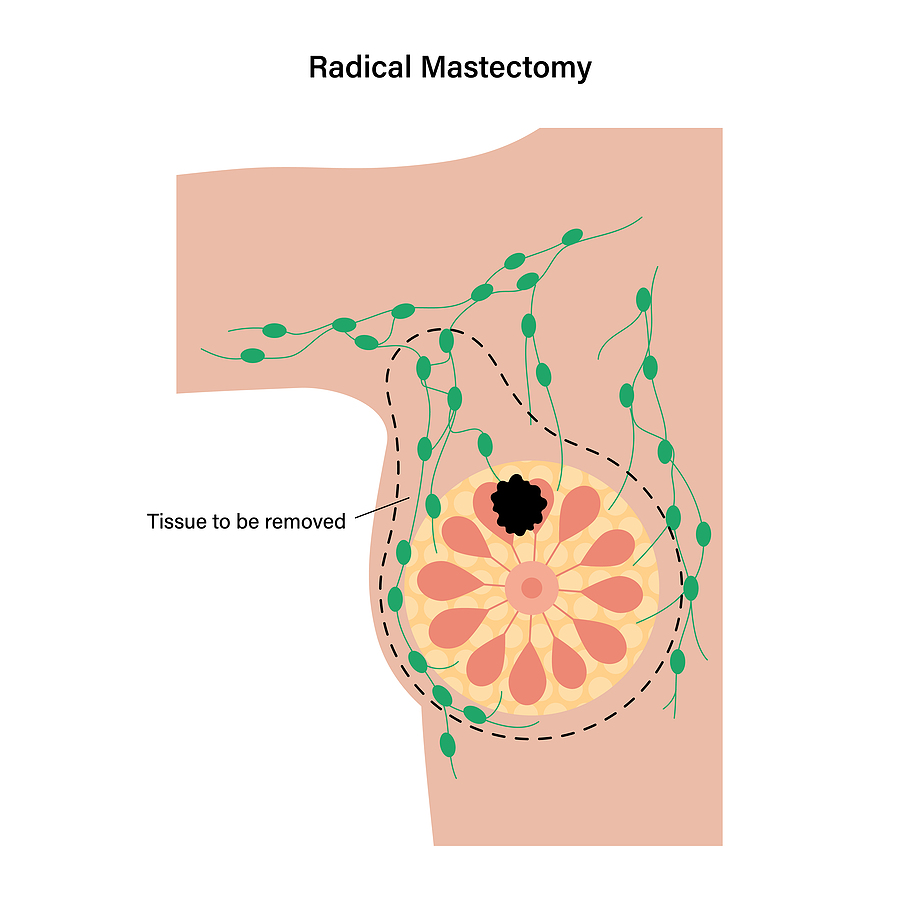
Persistent post-mastectomy pain (PPMP) is very common, so it has attracted much attention. Pain management after mastectomy is difficult to manage, as it is associated with social, psychological and functional issues. Radiation, lymph nodes resection, lymphoedema, tissue fibrosis are related to persistent pain. Sociodemographic factors, such as being in an ethnic minority, young age and also preoperative painful situations, favour PPMP. 6
Pain management demands a multimodal approach. Pickering et al7 proved the effect of memantine, a NMDA receptor antagonist on pain in animals. Reyad et al 8 administered 75mg pregabalin twice a day for a week, starting from the morning of surgery, with reduced pain scores.
Esmolol is a selective, short-acting, β1-adrenoreceptor antagonist, which is metabolised by plasma esterase. Its properties as an anaesthetic adjunct is unknown and it acts both peripherally and centrally. Cautious use is demanded in cases of renal insufficiency, due to renal excretion of its metabolite. In doses between 50-300mcg/kg/min, its metabolism is independent of renal or hepatic function. Esmolol decreases heart rate and blood pressure and it is contraindicated in bradycardia, heart block greater than first degree, heart failure and cautious use is crucial in diabetes and bronchospasm. In comparison with other non-opioid analgesics, esmolol shows similar results to lidocaine and less sedated patients. 9 Not only this, but it offers haemodynamic stability after surgery.10
In conclusion, multimodal pain treatment after mastectomy needs serious attention. Preoperative factors should be identified, psychological issues should be addressed and pain management should include a variety of medications, as mentioned above. Esmolol, in doses mentioned, offers important advantages and with an elimination half-life of 9 minutes, its effects are both rapid and transient. By reducing opioids, less sedation and PONV and faster patient discharge are noticed. 11Esmolol seems to act as a promising adjunct, though more clinical trials should be carried out in order to produce more reliable results.
References
- Mendonça, F T.; Tramontini, A J.; Miake, H I et al. Eur J Anaesthesiology 2021;38:735 doi: 10.1097/EJA.0000000000001512
- Watts R, Thiruvenkatarajan V, Calvert M, et al.. J Anaesthesiol Clin Pharmacol 2017; 33:28
- Gelineau AM, King MR, Ladha KS, et al. AnesthAnalg 2018; 126:1035 – 1049.
- King CA, Perez-Alvarez IM, Bartholomew AJ, et al.. Breast J. 2020;26:1742. doi: 10.1111/tbj.13999
- DinhKH, McAuliffe PF, Boisen M, et al. Ann Surg Oncol. 2020;27:4828. doi: 10.1245/s10434-020-08880-1
- Tait R, Zoberi K, Herndon C, J Pain, 2018; 19:1367
- Pickering G, Morel V, Joly D, et al. Trials. 2014;15:3317
- Reyad RM, Omran AF, Abbas et al. J Pain Symptom Manage. 2019;5:1
- Bajracharya JL, Subedi A, Pokharel K, et al BMC Anesthesiol. 2019;191:198.
- Vahabi S, Rafieian Y, Abbas Zadeh A. J Invest Surg. 2018;3:82
- Harless M, Depp C, Collins S,et al. AANA J. 2015;83:167
Read our Monthly newsletter.
Read More of our special newsletter covering our virtual congress 2020.
Visit our COVID-19 Resource Hub for other news and resources.










