Newsletter 2025
The SAFEST project
How does it trigger patient safety?
What is the SAFEST project?
The SAFEST calls for improving quality and patient SAFEty in surgical care through Standardisation and harmonisation of perioperative care in Europe. It arose in response to a critical need: the high incidence of surgical adverse events in Europe, affecting between 8% and 12% of hospitalised patients. To address this situation, SAFEST seeks to provide a framework to improve patient safety in the perioperative period through the development and implementation of standardised, evidence-based practices, with a strong patient-centred approach.
The Perioperative Patient Safety Recommendation Consensus
The SAFEST project was based on an initial consensus: 101 evidence-based recommendations that followed a rigorous methodology combining systematic review, multidisciplinary consensus, and in-person validation:
- First, a systematic review1 of 267 clinical practice guidelines yielded 4,666 individual recommendations, of which 2,095 were supported by moderate or strong evidence. These were synthesised into 99 preliminary recommendations.
- Second, a multidisciplinary Delphi process, involving 66 experts from 19 European countries — including clinicians, nurses, managers, quality experts and patient representatives— evaluated the drafts in terms of clinical relevance and feasibility. Recommendations that reached at least 70% agreement in both dimensions were retained.
- Third, a consensus conference refined and validated the recommendations, resulting in a final set of 101 practical, evidence-based, patient-centred, perioperative patient safety recommendations.
- As a fourth step, the recommendations were further refined and translated following external review and real-life application through the follow-up through the SAFEST protocol2, as explained below.
These 101 recommendations 3 were organised into 12 thematic areas covering the entire perioperative pathway, from preoperative assessment to discharge and continuous system improvement. They represent a roadmap for perioperative practice that all should aspire to. They represent a valuable resource, providing an entire curriculum for patient safety in the perioperative period, a standard to be audited against, and potentially a driver for improvement in patient safety 4.
To facilitate the diffusion of this enormous effort, the idea of the Compass emerged: a visual guide to oversee the 101 recommendations, designed to eventually help hospitals navigate this compendium and chart their own path through patient safety improvement. This tool may enable each institution to adapt the journey according to its needs, priorities, and resources, thus promoting a personalised and sustainable transformation.
The SAFEST patient safety Compass is openly available through a digital and interactive website. It also includes a “lay language” section, presenting the same information in a less technical, more accessible format so that any user, regardless of background, can fully understand it. Additionally, the recommendations can be downloaded individually or as a complete set, and are available in multiple languages, allowing for adaptation to the linguistic preferences of each user.
From the Perioperative Patient Safety Recommendations to quality improvement through the patient safety self-evaluation.
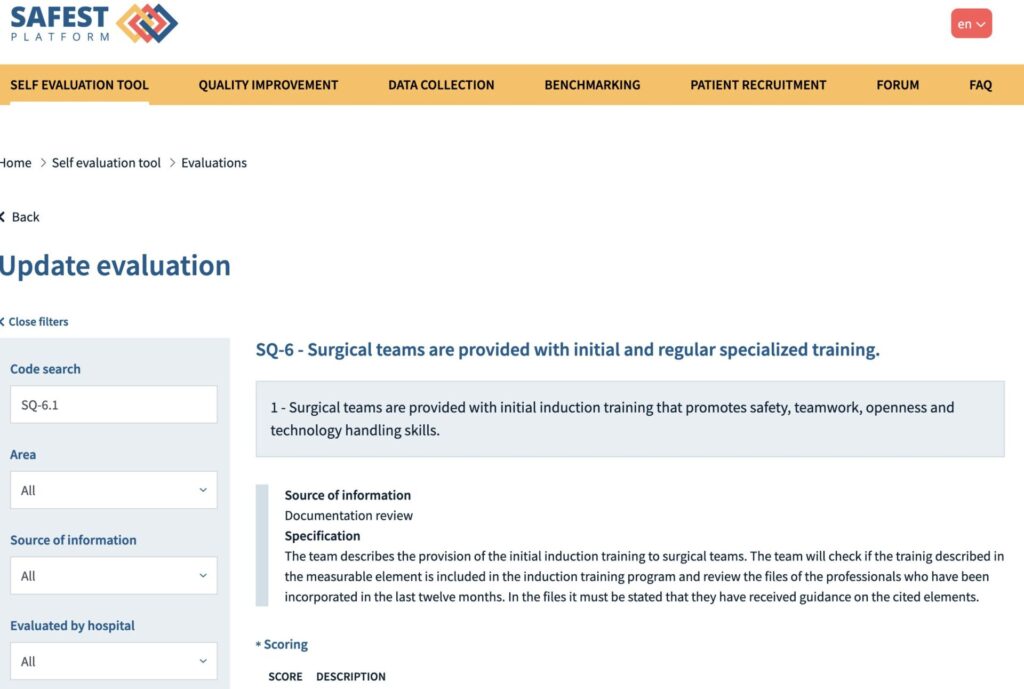
Following the consensus, the next challenge was to evaluate the state of the recommendations implementation in ten hospitals distributed in five European countries. To this end, the recommendations were transformed into measurable and practical standards, which were embedded into an online self-evaluation tool that enabled hospitals to assess their adherence to best practices. A multidisciplinary team, including anaesthesiologists, surgeons, nurses, quality officers, hospitalists, IT specialists and patients, followed a five-day diagnostic plan with the support of the SAFEST research team. An online SAFEST self-evaluation tool served as a powerful diagnostic instrument, allowing institutions to identify strengths, gaps, and opportunities for improvement in perioperative care (Figure 1). The self-evaluation was performed following a common manual, through an estimated five-day program effort. It was not an accreditation, but a means to gather the intelligence to depict a comprehensive picture of the patient safety strategies implemented in every hospital; therefore, it was based on mutual trust between the research team and the hospital teams. Confidential and anonymous benchmarking was available for informative purposes (Figure 2).

Prioritisation and action planning in the 10 implementing hospitals
The next step in the project was to establish improvement priorities and develop action plans to improve patient safety in perioperative care across hospitals and their care networks.
Instructional materials with selection criteria (e.g. common low scores in the self-evaluation results) were created to guide hospitals in setting tailored improvement priorities. These materials were shared and discussed with the consortium partners and piloted in the hospitals.
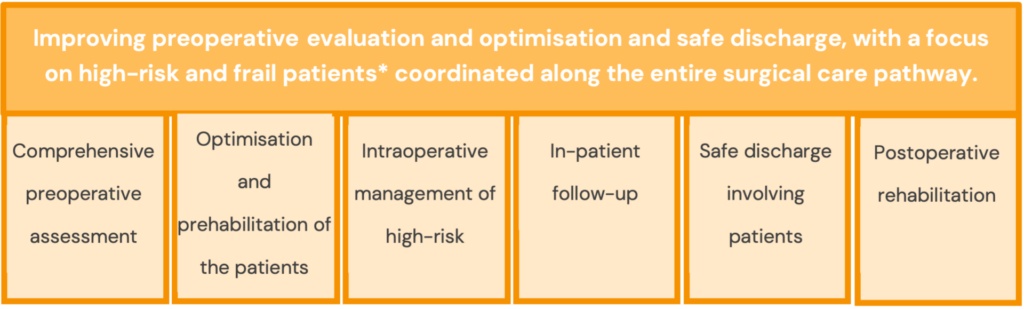
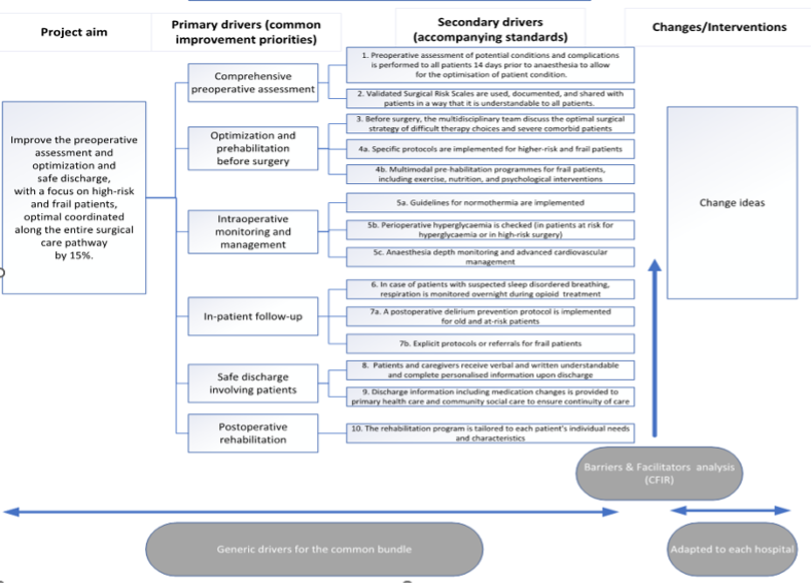
Applying the selection criteria, six common improvement areas were determined: Comprehensive preoperative assessment; Optimisation and rehabilitation before surgery; Intraoperative monitoring and management; In-patient follow-up; Safe discharge involving patients; and Postoperative rehabilitation, with a focus on high-risk and frail patients (Figure 3).
Then, a generic driver diagram (DD) was developed to visualise key change drivers and context-specific barriers (Figure 4). This diagram was developed and provided to the hospitals to facilitate the translation of the common improvement areas into concrete change ideas and action plans. It was supplemented with a structured barrier analysis to get a complete picture of determinants that may hinder or facilitate the implementation of the standards in the common improvement areas. The Consolidated Framework for Implementation Research (CFIR) was used to guide this step. Several activities were organised at the hospital to adapt the common bundle to local contexts: a training webinar, one-on-one online meetings with hospital teams and a live workshop held in the Military University Hospital, Prague (April 2024). This hands-on session helped finalise the driver diagrams and develop hospital-specific action plans, ready for implementation and further discussion in the Learning Community.
Action plans and toolbox development
Finally, a comprehensive toolbox was developed, including:
- Criteria for selecting individual improvement aims
- Templates for driver diagrams and action plans
- A 14-item measurement tool for barrier and facilitator analysis, based on CFIR determinants
- A list of effective safety interventions from the umbrella review
- Results from the prioritisation process in the 10 pilot hospitals (the common bundle with shared improvement priorities)
The toolbox may provide structured guidance to:
- Select improvement priorities (from the common bundle or locally defined)
- Identify and prioritise key determinants (barriers and facilitators)
- Develop and monitor action plans with concrete change ideas
- Choose promising interventions from a robust evidence base to enhance perioperative patient safety
Working together for safer surgery: The SAFEST learning collaborative
At the centre of the SAFEST project lies the Perioperative Quality Improvement Learning Collaborative (PQILC)—a structured approach that brings together hospitals across Europe to work on shared goals in surgical safety and quality improvement.
The collaborative connects the 10 above-mentioned hospitals’ multidisciplinary teams working side by side as equal partners. This diversity ensures that improvement efforts are informed by clinical expertise, technical insight, and, importantly, the patient perspective.
To foster progress, the collaborative is organising learning sessions where teams exchange lessons learned and share best practices, to work on their improvement projects. Progress is meant to be tracked through self-evaluation tools, data collection5, and benchmarking on the SAFEST platform to allow hospitals to monitor their adherence, learn from one another, and celebrate improvements. At the same time, the collaborative explores the broader context—looking at the barriers and facilitators at different levels of the health system that can influence both implementation and long-term sustainability.
In this way, the Learning Collaborative acts as a dynamic engine for change, helping hospitals move beyond isolated initiatives toward lasting, patient-centred improvement in perioperative care.
Patients at the heart of SAFEST
Patients are not just participants but true partners in SAFEST. From the very start, they have helped shape a shared European vision for safer surgical care. Through a dedicated Patient Advisory Board, interviews across participating hospitals, and active involvement of a patient researcher in defining meaningful outcomes, patients ensure that the standards we develop reflect what really matters to them. By working side by side with clinicians and researchers, their experiences and perspectives guide the Learning Collaborative, making perioperative safety improvements more relevant, credible, and sustainable.
By actively incorporating patients’ voices, SAFEST ensures that safety practices and outcome measures reflect what matters to them, rather than what clinicians might assume on their own. Patient involvement not only enhances the relevance of the project but also increases its credibility: practices co-designed with patients are more likely to be embraced and sustained by both healthcare teams and patients themselves. Moreover, by engaging patients in defining the outcomes, SAFEST creates benchmarks that are grounded in real experiences, leading to more meaningful, patient-centred evaluation and monitoring. One example of this collaboration is the SAFEST patient empowerment video, which encourages patients to speak up during their perioperative journey.
What is the opportunity for hospitals in Europe and Beyond?
We are thrilled to announce that the SAFEST self-evaluation tool is now open to hospitals across the EU and beyond. By participating, institutions will have the opportunity to evaluate and strengthen their perioperative safety practices, receive personalised feedback and expert guidance, benchmark their performance against peers, and benefit from training webinars and a user-friendly digital platform. Most importantly, they will join a growing community of hospitals committed to shaping the future of surgical safety. Hospitals interested in participating are warmly invited to watch this informative video and sign up through the SAFEST registration form, or contact us at fad@fadq.org for further information.
Authors:
- Carola Ayuso. SENSAR researcher. Valencia
- Claudia Valli, SAFEST Project Manager. Fundacion Avedis Donavedian, Barcelona.
- Hiske Calsbeek. Radboud University Hospital senior researcher. Nijmehen
- Caroline Schlinkert, senior researcher at the Netherlands Institute for Health Services Research (Nivel). Amsterdam.
- Daniel Arnal-Velasco *(Corresponding author). ESAIC honorary member, FESAIC, PSQC member. SENSAR Researcher. Head of Surgical Process, Hospital Universitario Fundacion Alcorcon. Associate Professor at King Juan Carlos University. Madrid. darnal@sensar.org
- Anita Heideveld-Chevalking, coordinator perioperative patient safety and senior researcher at Radboud UMC
References:
- Martinez-Nicolas I, Arnal-Velasco D, Romero-García E, et al. Perioperative patient safety recommendations: systematic review of clinical practice guidelines. BJS Open. 2024 Oct 29;8(6):zrae143. doi: 10.1093/bjsopen/zrae143.
- Valli C, Schäfer WLA, Bañeres J, et al. Improving quality and patient safety in surgical care through standardisation and harmonisation of perioperative care (SAFEST project): A research protocol for a mixed methods study. PLoS One. 2024 Jun 13;19(6):e0304159. doi: 10.1371/journal.pone.0304159.
- Arnal-Velasco D, Martinez-Nicolas I, Fabregas N, et al. Multidisciplinary, evidence-based, patient-centred perioperative patient safety recommendations: a European consensus study. Br J Anaesth. 2025 Sep;135(3):723-736. doi: 10.1016/j.bja.2025.04.047
- Weller J, Scot D. Using perioperative patient safety guidelines to drive systems change. Br J Anaesth. 2025 (in press). doi: 10.1016/j.bja.2025.06.023.
- Dinis-Teixeira JP, Nunes AB, Leite A, et al. Moving towards a core measures set for patient safety in perioperative care: An e-Delphi consensus study. PLoS One. 2024 Oct 23;19(10):e0311896. doi: 10.1371/journal.pone.0311896.