Newsletter 2025
A Short History of Anaesthesia Before 1846
The modern era of anaesthesia officially began on 16 October 1846, when dentist William Morton (1819 – 1868) and surgeon John Warren (1778 – 1856) made history at Massachusetts General Hospital by successfully using diethyl ether to prevent pain during surgery to remove a lump under the jaw of patient Gilbert Abbott (1825 – 1855). However, the human desire to alleviate pain predates this landmark event by millennia. Artifacts and ancient writings trace early anaesthesia attempts back to around 4000 BC. Sumerian artifacts depicted the opium poppy, and ancient texts describe various methods to ease pain, often through the ingestion of ethanol or herbal mixtures.
These early anaesthetics were developed in regions where mind-altering plants like opium, henbane (Hyoscyamus Niger), mandrake, and coca leaves were native. The Chinese physician and surgeon Hua Tuo (ca. 111 – 207 AD) is known to have used a herbal anaesthetic made from hemp and wine, called “mafeisan.” Throughout the centuries, sedative mixtures continued to be developed. The Swiss physician Theophrastus Von Hohenheim, better known as Paracelsus (1490–1541), experimented with various opium concoctions, and the London Pharmacopeia (1618) mentioned laudanum – a pill made from opium, saffron, castor, ambergris, musk, and nutmeg. In 1676, the English physician Thomas Sydenham (1624–1689) simplified this recipe by using only opium and alcohol.
The concept of inhalational anaesthesia dates back to before 1846. Ibn Sina (980–1037), known as Avicenna, was a Persian physician and philosopher who described sedative inhalation for surgery in his book The Canon of Medicine. He noted that Arabic physicians used a “soporific sponge” soaked in an herbal potion, which was placed under a patient’s nose to induce unconsciousness during surgery. This technique was further developed in Western medicine by the Salerno School of Medicine in the late 12th century, particularly by the Italian surgeon Ugo Borgognoni (Hugh of Lucca: 1160 – ca. 1259). The sponge was described and promoted by Hugh’s (presumed) son, surgeon Theodoric Borgognoni (Theodoric of Lucca: 1205 –1298). This type of anesthetic involved a sponge soaked in a dissolved solution of opium, mandragora, hemlock juice, and other substances, moistening it before surgery. Fennel roots and vinegar were used to wake the patient. The soporific sponge was used for centuries, even by the renowned French surgeon Ambroise Paré (1510 – 1590). However, by the late 16th century, this practice began to fade from medical texts. Possible reasons include its association with magical practices, the influence of the Roman Inquisition (1542), and the perception that it was ineffective for longer surgeries.
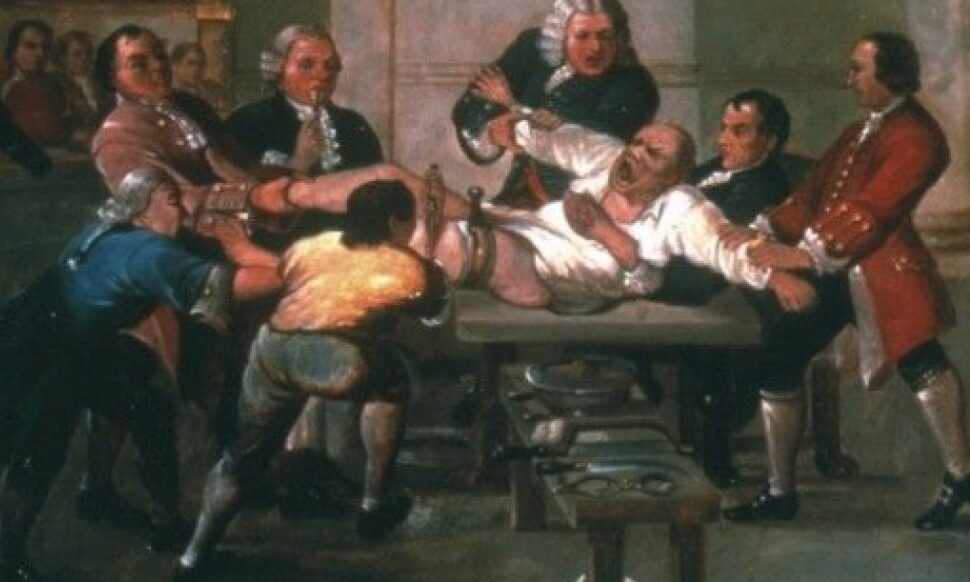
During the 17th and 18th centuries, surgeries were often performed without anaesthesia. Surgeons relied on alcohol, something for patients to bite down on, or simply the patient’s ability to withstand pain. However, all pictures and writings available from before 1846 show that mechanical immobilization of patients by different means was a central part of the surgical procedure. The first reliably recorded use of a general anaesthetic occurred in 1804 in Japan when physician Seishu Hanaoka (1760 – 1835) performed complex surgeries using a herbal mixture containing monkshood and thorn apple, which was consumed rather than inhaled. While his work was successful, it did not spread beyond Japan, and the world had to wait until 1846 for a successful demonstration of general anaesthesia using ether.
Interestingly, the discovery of ether dates back to 1275 AD, when the Catalan philosopher and alchemist Raymundus Lullus (1232 – 1315) first described it. It was later synthesized in 1540 by the Prussian botanist Valerius Cordus (1514 – 1554), who distilled sulfuric acid with fortified wine to create “oleum vitrioli dulce” (sweet oil of vitriol). Paracelsus recognized ether’s analgesic properties around the same time. Despite this early synthesis, ether was primarily used for recreational purposes for centuries.
Nitrous oxide was first synthesized in 1772 by the English chemist Joseph Priestley (1733 – 1803), and its analgesic properties were later noted by Humphrey Davy (1778–1829). The gas was primarily used for public entertainment until Horace Wells (1815–1888) realized its therapeutic potential and attempted a public demonstration at Massachusetts General Hospital in 1845, which unfortunately failed. This setback and the introduction of new anaesthetics such as ether and chloroform temporarily overshadowed nitrous oxide’s potential.
Chloroform was first produced in 1831 almost simultaneously by Samuel Guthrie (1782 – 1848) in the USA and Eugène Soubeiran (1797 -1858) in France. While the narcotic effects of chloroform became widely known, reports of sudden deaths due to its use soon emerged. Nonetheless, chloroform became widely used as an anaesthetic, especially between 1865 and 1920 in the United Kingdom and German-speaking countries, despite less enthusiasm in America.
Other methods of pain relief were explored in the past. In the 16th and 17th centuries, surgeons used nerve compression and mixtures of snow and ice for local anaesthesia. In 1766, the Viennese physician Franz Anton Mesmer (1734 – 1858) introduced “mesmerism” (which later developed into hypnosis), where patients under hypnosis became insensitive to pain. Acupuncture, a key component of traditional Chinese medicine, had been practiced in China as early as 1600 BC. In 1656, Christopher Wren (1632 – 1723) and Robert Boyle (1627 – 1691) pioneered intravenous therapy by injecting opium into a dog’s vein. A human death from a blood transfusion in France around 1667 led rapidly to a cessation of attempts at intravenous therapy in patients. When the injection of opium or morphine was eventually taken up, it was following the design of an effective syringe and needle by the Scottish physician Alexander Wood ( 1817 – 1884) in 1853.
By the mid-18th century, anaesthesia was becoming increasingly used for complex surgeries, but opposition to its use persisted, particularly in academic circles. In 1849, French physiologist François Magendie (1783–1855) argued that pain was a vital force essential for health and recovery and that anaesthesia would weaken this force. The same year, the American physician John Pollard Harrison (1796 – 1849), who was also a professor of pathology at the Medical College of Ohio and Vice-President of the American Medical Association, made the following statement: “Pain is curative – the actions of life are maintained by it – were it not for the stimulation induced by pain, surgical operations would more frequently be followed by dissolution”. In 1852, the United States Army surgeon, John Porter (ca. 1810 – 1869) stated: “Inhaling ether vapor in doses adequate to induce insensibility is highly dangerous. It tends to poison blood, impair muscle contraction, adversely affect the nervous system, and put wounds in an unfavourable state for recovery”. Finally, also the American obstetrician and chair of the Department of Obstetrics and Diseases of Women at Jefferson Medical College, Charles Delucena Meigs (1792 – 1869), was a lifelong opponent of anesthesia. Meigs believed that labour pains are “a most desirable, salutary and conservative manifestation of the life force“. Writing in 1856, he warned against the morally “doubtful nature of any process that the physicians set up to contravene the operations of those natural and physiological forces that the Divinity has ordained us to enjoy or to suffer“.
Despite such opposition, anaesthesia eventually became a cornerstone of modern medicine, revolutionizing surgery and pain management. Since 1846, anaesthesia has evolved significantly, with advancements continuing to shape the field. The history of how anaesthesia has developed since 1846 is, however, very country-specific, and in the upcoming newsletters, ESAIC has the intention to provide an update on how anaesthesiology has developed in every ESAIC member country.
References
- https://www.umhs-sk.org/blog/medical-milestones-discovery-anesthesia-timeline#:~:text=Early%20anesthesia%20can%20be%20traced,%5D%20for%20surgical%20pain%20relief%2C%22
- https://wfsahq.org/about/history/history-of-anaesthesia/
- https://www.hartfordstage.org/stagenotes/ether-dome/agony
- https://www.woodlibrarymuseum.org/history-of-anesthesia/
- J Wawersik History of chloroform anesthesia Anaesthesiol Reanim 1997; 22: 144 – 152.
- Juvin P, Desmonts JM.The Ancestors of Inhalational Anesthesia: The Soponic Sponges (XI – XVlltls Centuries). How a universally recommended medical technique was abruptly discarded. Anesthesiology 2000; 93: 265 – 269.
- Goerig M, Schulte am Esch J. History of nitrous oxide – with special reference to its early use in Germany. Best Pract Res Clin Anaesthesiol 2001; 15: 313 – 338.
- Dorrington KL, Poole W. The first intravenous anaesthetic: how well was it managed and its potential realized? Br J Anaesth 2013; 110: 7 – 12.
Author
- Stefan De Hert, MD, PhD, FESAIC, Emeritus Professor of Anaesthesiology, Faculty of Medicine and Health Sciences, Ghent University, Ghent, Belgium










